Macronutrients and water are necessary products that fuel the body’s daily processes. This chapter defines what an essential nutrient is, how macronutrients function in the human body as well as hydration requirements and ways to make sure clients maintain the proper fluid intake.
Introduction to Macronutrients
Nutrients
Nutrients are defined as chemical structures found in foods that are necessary for human life and the growth, maintenance, and repair of body tissues.1 The main nutritional constituents of food are proteins, fats, carbohydrates, vitamins, and minerals.
Essential Nutrients
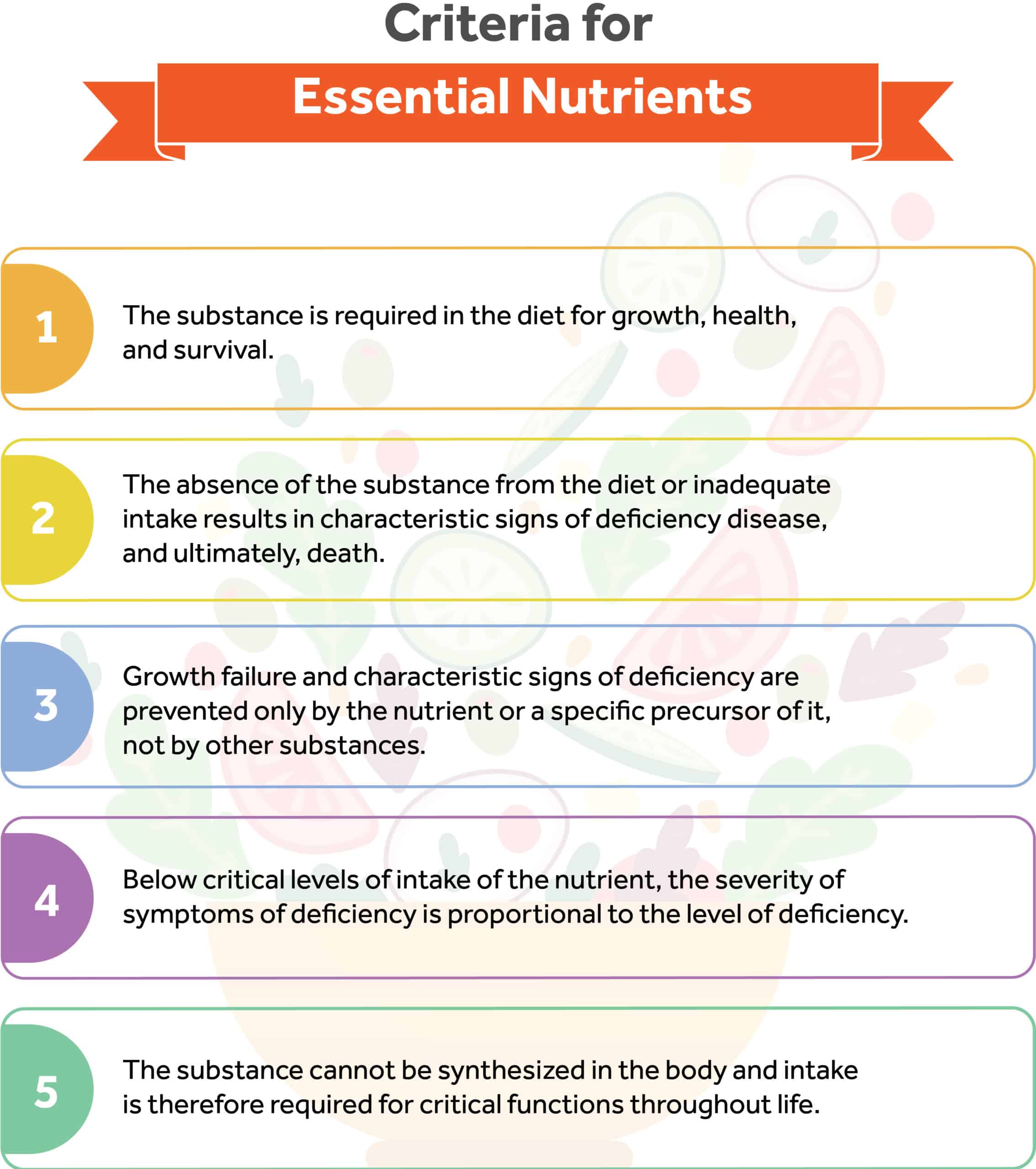
The search for the nutrients considered essential for health began in the late 1950s. Scientist Alfred E. Harper first defined and summarized them in 1999.1 The definition for essential nutrients includes several aspects.
Firstly, the substance is required in the diet for growth, health, and survival. Without it, or without the proper amounts of it, human beings exhibit signs of deficiency, disease, and ultimately, death. For example, salt is required for life. It is essential for nerve and muscle functions and helps regulate regulate fluids in the body. It is critical.
Another part of the definition for essential nutrients includes the fact that growth failure and characteristic signs of deficiency are prevented only by the nutrient or a specific precursor of it, not by other substances. So only this substance or a precursor to it will prevent signs of deficiency. Arginine is a non-essential amino acid that has many profound effects, but can actually be synthesized from other nutrients rather than just arginine or a precusor.
The human body cannot simply synthesize essential nutrients from other substances.
Also, below critical levels of intake of an essential nutrient, growth response, and severity of signs of deficiency are always proportional to the amount consumed, meaning a larger deficiency will lead to further and further symptoms and issues.
Examples of essential nutrients include certain carbohydrates, protein, fats, certain vitamins, minerals, and water.
Conditionally Essential Nutrients
With increasing scientific knowledge of human nutrition, came the understanding that some nutrients are not essential to maintain life. Defined as conditionally essential or indispensable, nutrients are the substances that partly meet the criteria for essentiality yet are not required in the diet.1 The only exception to the norm is specific populations that do not synthesize them in adequate amounts.
Non-Essential Nutrients
Non-essential nutrients are substances that cannot be synthesized by the human body but may be included in the diet given their significant effect on health, although the body can survive without them. Examples of non-essential nutrients include biotin, vitamin K, cholesterol, dietary fiber, certain amino acids, and fatty acids.
Macronutrients
Macronutrients are carbon compounds derived from food sources that provide the essential energy for growth, maintenance, metabolic functions, and survival. The three main sources of macronutrients include carbohydrates, proteins, and fats. Alcohol can be considered an alternative macronutrient because it is its source of energy but it is not essential for survival.
Energy Content and Structure of Macronutrients
Energy
Energy can be defined as the strength and vitality required for sustained physical or mental activity. The sun is the main source of energy for all living organisms and is primarily used by photosynthetic organisms such as plants, algae, and cyanobacteria to make carbon matter from carbon dioxide and water.3 Human beings require the use of this energy for building metabolic substances and components that are essential for growth and survival.
The energy that food produces is directly measured by calorimetry. In chemistry and thermodynamics, calorimetry is the science that measures the amount of heat that is transferred by burning a sample of food mass. In biological systems energy in foods is measured in kilocalories (kcal) or kilojoules (kJ). One kilocalorie (equivalent to 4.184 kJ) is the amount of heat required to raise the temperature of 1 kg of water to 1°C at standard atmospheric pressure of 760 mm Hg.4 To simplify the following formula, the field of nutrition uses kilocalories and calories interchangeably and defines 1 Kcal = 1,000 cal or 1 large calorie.
The three main macronutrients individually provide a relative energy content that can be measured by kilocalories per gram. Carbohydrates and proteins provide us with 4 kcal per gram and fats with 9 kcal per gram. Alcohol is not a nutrient but provides 7 kcal per gram as usable energy.
Certain nutrients require more energy to digest than others, which reduces the net energy supplied by the nutrient. Fiber, for example, requires significant energy to digest. As a carbohydrate, fiber technically has 4 calories per gram. However, the net digestion requirements result in roughly 2 calories acquired per gram. Overall, the net energy or caloric value of a food is the energy that is supplied to the body after each nutrient has been metabolized.
Carbohydrates
Functions
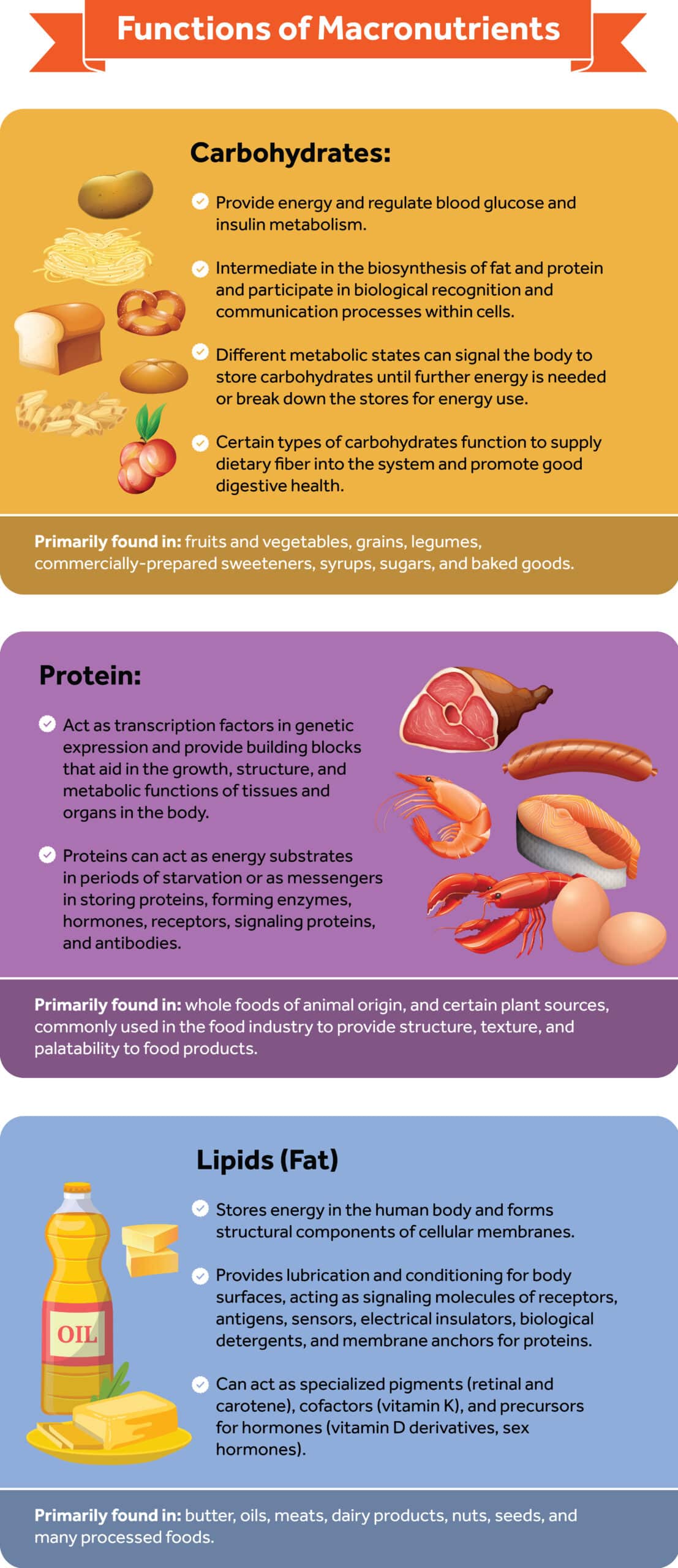
Carbohydrates are the most abundant organic compound in food and the major energy source for humans, supplying half or more of the total caloric intake for many.5 Carbohydrates exist as large molecules in the cell walls of bacteria, plants, and the connective tissues of animals to maintain structure and protection.6 The principal role of carbohydrates is to provide energy and regulate blood glucose and insulin metabolism.7
Carbohydrates also function as metabolic intermediates in the biosynthesis of fat and protein and participate in biological recognition and communication processes within cells.7 Different metabolic states can signal the body to store carbohydrates until further energy is needed or break down the stores for energy use.
Certain types of carbohydrates also function to supply dietary fiber into the system and promote good digestive health. Carbohydrates are primarily found in fruits and vegetables, grains, legumes, commercially-prepared sweeteners, syrups, sugars, and baked goods.
Structure and Properties
Carbohydrates are structurally made from carbon (C), oxygen (O), and hydrogen (H) atoms. The general chemical structure for carbohydrates is (CH2O)n where n is the number of carbons in the molecule.8 Carbohydrates can be classified into two major classes: simple carbohydrates and complex carbohydrates depending on the number of sugar molecules in the structure. Simple carbohydrates include monosaccharides (1 single sugar unit), and disaccharides (<2 sugar units). Complex carbohydrates include oligosaccharides (3–10 sugar units) and polysaccharides (>10 sugar units).
Simple Carbohydrates
Monosaccharides, also termed simple sugars, are the basic units from which all carbohydrates are built. Monosaccharides differ from complex carbohydrates in that they are colorless crystalline structures with a sweet taste, solid at room temperature, and soluble in water.8 Simple carbohydrates are classified using numerical prefixes (tri-, tetra-, penta-…) according to the number of carbon atoms.8 Following this rule, monosaccharides with three carbons are called trioses, those with four are carbons tetroses, those with five are carbons pentoses, and so forth. The most abundant monosaccharide in nature and most important nutritionally is glucose, a six-carbon sugar.8 Other common monosaccharides found in foods include fructose and galactose.
Disaccharides are composed of two monosaccharides covalently linked by glycosidic bonds. Disaccharides can be readily broken down (hydrolyzed) or reduced to their constituent monosaccharides by acidic or enzymatic reactions.8 Similar to monosaccharides, disaccharides are also colorless crystallized structures with a solid appearance.8 The most significant structures in this group are sucrose, lactose, and maltose as summarized below:
- Sucrose: also known as table sugar, is a sugar present in fruits and vegetables, predominantly sugarcane. Sucrose consists of one glucose and one fructose molecule and is represented by the molecular formula C12H22O11. Sucrose is characterized by being highly soluble in water and sweeter than its constituent disaccharides.8 The functional property of the former is partially influenced by fructose, the monosaccharide with the highest content of sugar. This is why sucrose is widely extracted to be used as a sweetening agent and to form syrups and nectars.
- Lactose: is the only sugar that is biologically made in the body, particularly in the breast milk of lactating mammals. This disaccharide is present in dairy products like milk and cheese and commercially manufactured for pharmaceutical products and infant formulas. Consisting of one glucose and one galactose molecule, lactose is also represented as C12H22O11, however, it is less sweet and soluble than sucrose.8 Compared to milk from other mammals, human milk is considered unique in its high sugar content; it contains about 70 g/L lactose (7%) contributing to around 40% of the caloric value.9
Lactose intolerance is the deficiency or reduced activity of lactase enzymes in the small intestine that develops in some people after the consumption of milk or milk products. When lactose-containing products are consumed, the undigested lactose remains in the gut. As the bacteria in the large intestine ferment lactose, they produce hydrogen, methane, and carbon dioxide gas that causes bloating and abdominal pain. The presence of unabsorbed lactose and products of fermentation causes an increase in osmotic pressure, attracting water into the bowels, so water flows in and leads to diarrhea.
- Maltose: is the most limiting sugar found in nature and is rarely consumed in the diet. Sources of maltose include germinated seeds of plants and grains that are kept in water for a long time.8 Maltose is a disaccharide that is made of two glucose molecules and also shares the same molecular formula as that of lactose and sucrose (C12H22O11). Similar to its constituents, maltose is sweet and soluble in water.
Complex Carbohydrates
- Oligosaccharides are carbohydrate polymers that link three to 10 simple sugars by glycosidic bonds. Oligosaccharides are not as abundant as disaccharides except for maltodextrins and raffinose.8 Maltodextrins are used in many commercially prepared foods as thickeners, sweeteners, humectants, and corn syrup, whereas raffinose, also known as “flatulence sugar” is naturally found in legumes and can lead to excessive flatulence as a result of gut bacteria fermentation.10
- Polysaccharides are carbohydrate polymers composed of over 10 sugar units that exist in linear or branched formations. The properties of polysaccharides depend on their chemical and conformational structures. In general, highly branched polysaccharides are water soluble and form relatively nonviscous solutions, whereas linear polysaccharides tend to be insoluble in water and form viscous solutions.8
Polysaccharides exist as starch, glycogen, cellulose, and hemicellulose and are classified based on how readily digestible they are in the human body. The major digestible polysaccharides are starch, stored mainly in plant cells, and glycogen, stored solely in animal tissues, particularly in the liver and muscle.8 Plants also synthesize polysaccharides that are non-digestible in the human gut such as cellulose, hemicellulose, and pectin.
Protein
Functions
Proteins are the most abundant macronutrient in the body that virtually exists in every cell, with over 40% of body protein found in skeletal muscle, over 25% found in body organs, and the rest found mostly in the skin and blood.8 Proteins are virtually involved in every process that takes place in cells.
The principal functions of proteins are to act as transcription factors in genetic expression and to provide building blocks that aid in the growth, structure, and metabolic functions of tissues and organs in the body.7 More specifically, proteins can act as energy substrates in periods of starvation or as messengers in storing proteins, forming enzymes, hormones, receptors, signaling proteins, and antibodies.7 Proteins are present in whole foods of both plant and animal origin and used in the food industry to provide structure, texture, and palatability to food products.
Amino Acid Classification
Amino acids are units of protein in their simplest form made of a central carbon (C) that bonds at least one amino group (-NH2), at least one carboxyl group (-COOH), and a side chain (R group). Amino acids can be classified based on structure, net charge, polarity, and essentiality. What makes protein functions unique is the R group, a side chain that can take on many different chemical forms and is configured from one of the 20 amino acids that every human body requires to function.8
In 1957, William C. Rose and his colleagues defined a system of categorizing amino acids based on essentiality.11 Out of the hundreds of amino acids that the body can build, only nine amino acids are considered essential or indispensable.11 In other words, essential amino acids cannot be synthesized by the body and therefore must be supplied by the diet. The following list identifies the amino acids that are essential from those that are not essential.11

Peptides and Proteins
Proteins are chains of over 50 amino acids that fold into three dimension configurations. Similar to carbohydrates, amino acids form chains of various lengths held together by amide bonds, and named after the number of molecules in the chain. A polypeptide is a single linear chain made of many amino acids, and an oligopeptide is a chain of 2-20 amino acids.8
The naming of oligopeptides uses a similar approach to monosaccharides by using numerical prefixes (di-, tri-, tetra-, penta-...) to determine the size of the polymer.8 For example, two amino acid molecules can be covalently joined to yield a dipeptide, three amino acids can be joined to form a tripeptide, four amino acids can be linked to form a tetrapeptide, and so forth.8
Lipids
Functions
Lipids, also referred to as fats, account for 30% to 35% of total caloric intake for many.5 The primary function of lipids is to store energy in the human body and form structural components of cellular membranes.7 Other important functions of lipids include providing lubrication and conditioning for body surfaces, acting as signaling molecules of receptors, antigens, sensors, electrical insulators, biological detergents, and membrane anchors for proteins.7
Lipids can act as specialized pigments (retinal and carotene), cofactors (vitamin K), and precursors for hormones (vitamin D derivatives, sex hormones).8 Dietary sources of lipids predominantly exist as triacylglycerols (TAGs) in butter, oils, meats, dairy products, nuts, seeds, and many processed foods. Fats are commercially used as a cooking medium, to increase the tenderness of baked goods, and add richness and flavor to meals.
Structure and Properties
Lipids are structurally composed of carbon (C), hydrogen (H), and oxygen (O), but unlike carbohydrates, they are insoluble in water. The capacity to classify lipids is limited to their solubility property given that the systematic organic chemical naming of lipid structures is dominated by trivial names.8 Lipids can therefore be classified based on the products of synthesis and their structural and functional similarities.
Triacylglycerols (TAGs) are virtually the most abundant storage form of lipids in the adipose tissue and account for nearly 95% of dietary fat. The structure of TAGs is composed of a glycerol backbone to which three fatty acids are attached by ester bonds.8 The three fatty acids can be saturated (SFA), monounsaturated (MUFA), polyunsaturated (PUFA), or a combination.8
Fatty acids are single fat molecules composed of a soluble carboxylic acid head and an insoluble hydrocarbon acid chain tail. Fatty acids are classified according to the length of the hydrocarbon chains and their degree of saturation. Typically short-chain fatty acids chains have fewer than 6 carbon atoms, medium-chain fatty acids have 8 to 14 carbons, and long-chain fatty acids have more than 14 carbons.8 Fatty acids can also be classified as unsaturated or saturated depending on the number of double bonds in the hydrocarbon chain.
- Trans Fatty Acids are chains of fat characterized by trans geometric bonds between a double bond. The degree of bonding plays an important role in the structure and function of cell membranes. The more carbon-carbon cis double bonds a chain has, the more pronounced the bonding effect.8 Trans fatty acids are mainly produced as a result of partial hydrogenation.8 Partial hydrogenation is the process commonly used to make frying oils and commercial food products remain solid at room temperature. The role of trans fatty acids in the etiology of cardiovascular disease is well established in the literature, indicating the potential risks associated with the consumption of trans fatty acids in the human diet.12
- Unsaturated Fatty Acids are chains of fat molecules with at least one double bond. The main property of these fats is their ability to stay liquid at room temperature based on their double bond configuration.8 Unsaturated fats exist as monounsaturated fatty acids (MUFAs) and polyunsaturated fatty acids (PUFAs). MUFAs such as oleic acid (C18:1, ω-9) are considered omega-9 fatty acids (C18:1, ω-9) and are not essential in the diet.8
Sources of MUFAs include vegetable oils like olive, avocado, canola, peanut, and sesame oil. PUFAs such as linoleic and linolenic acid are essential in the diet because the body cannot synthesize them. Linoleic acid (C18:2, ω-6) is an omega-6 fatty acid that primarily exists as arachidonic acid (ARA) and can become inflammatory if consumed in a high amount.
Food sources of omega-6s are corn, soybean, and safflower seed oils. Linolenic acid (C18:3, ω-3) is an omega-3 fatty acid that appears to play anti-inflammatory roles in the prevention and treatment of chronic diseases.13,14 Chief among the omega-3 fatty acids are eicosapentaenoic acids (EPA), and docosahexaenoic acids (DHA), found in whole foods such as cold-water fatty fish, shellfish, and algae, respectively.
Phospholipids are composed of glycerol, phosphate, and the appropriate base, such as choline, and show similar solubility properties to fatty acids. Particularly, the soluble head group and insoluble fatty acyl chains allow phospholipids to form outer layer membranes, structural components of the brain and nervous tissue, membranes of body tissues, and lipoproteins.8 Phospholipids are classified based on their head group. The five major classes of phospholipids thus are phosphatidylcholine (PtdCho, also called lecithin), phosphatidylethanolamine (PtdEtn), phosphatidylserine (PtdSer), phosphatidylinositol (PtdIns), and phosphatidylglycerol.8 Phospholipids are found in sources of whole foods such as eggs, organ meats, lean meats, fish, shellfish, cereal grains, and oil seeds.
Cholesterol is a derivative of plant sterols that frequently exist in foods and body tissues esterified to one fatty acid per molecule. Similar to phospholipids, cholesterol is a membrane component essential in brain and nervous tissue formation.8
The main function of cholesterol is to form bile acids, steroid hormones, and the precursor to vitamin D.8 Cholesterol occurs naturally in foods of animal origin, mainly in liver and egg yolk, red meats, poultry, whole milk, and cheese. Dietary cholesterol, which was once thought to increase the risk of heart events, is no longer associated with heart disease, ischemic stroke, or hemorrhagic stroke, and in some cases, appears to improve lipoprotein particle profiles and HDL functionality.15
Digestion, Absorption, and Metabolism of Nutrients
The Gastrointestinal Tract
The gastrointestinal tract (GIT) or gastrointestinal system is the tubular structure that extends from the mouth to the anus. The GI system includes the oral cavity, pharynx, esophagus, stomach, small intestine, large intestine, and rectum, as well as accessory organs (salivary glands, pancreas, liver, and gallbladder) that provide essential secretions. The main functions of the GI are (1) digestion of carbohydrates, proteins, and fats from dietary sources, (2) absorption of fluids, micronutrients, and trace elements, (3) and providing immune protection against pathogens.16
Digestion, Absorption, and Excretion
Digestion
Digestion encompasses all the processes that result in the breakdown of macronutrients into smaller units. Digestion is assisted by mechanical (physical) and enzymatic (chemical) processes. Mechanical digestion includes chewing, mixing of food with secretions from the GIT, and contractility of the stomach and the intestines to allow passage and breakdown of the food.
The process of digestion and absorption of macronutrients begins in the mouth. The mechanical forces of the oral cavity cut and grind food and mix it with saliva to form a food bolus.16 The main role of saliva is to initiate the digestion of carbohydrates and fat, neutralize acids in the mouth, and assist in swallowing food.
Carbohydrates and fats are the only macronutrients that are initially digested in this site, with the aid of salivary amylase and salivary lipase, respectively. From the mouth, the food bolus is swallowed by passing from the pharynx into the esophagus. Swallowing is a voluntary reflex regulated by the brain.16
Once the bolus enters the stomach, the smooth muscles of the stomach, the gastric acid juices, mucosa, and enzymes facilitate the transformation of the bolus into a chyme.16 The gastric juice is highly acidic and creates an acidic environment for carbohydrates, lipids, and protein to break down. Proteins are broken down into smaller peptides by pepsin, an enzyme that is activated by the hydrochloric acid in the gastric juice. Lipids containing triacylglycerols (TAGs) are hydrolyzed first into diglycerides and then fatty acids by the enzyme gastric lipase. Carbohydrates are further broken down by salivary amylase until it is inactivated by the low pH of gastric juice.
Absorption
Absorption is the movement of nutrients, including water and electrolytes across the mucosal lining of the GIT into the blood or the lymphatic system.16 The main organ responsible for complete digestion and absorption is the small intestine, which accounts for specialized absorptive cells that increase the uptake of nutrients across the extracellular compartment.
Once the stomach has acidified the chyme, it enters the small intestine where it is completely absorbed. The small intestine is composed of three sections, the duodenum, the jejunum, and the ileum. Absorption is accomplished by structural components called villi and microvilli, hair-like extensions that project out of the lumen of the intestine and are made of absorptive cells to transport nutrients out into the blood.16
When predigested macronutrients enter the small intestine, the pancreas releases pancreatic juice and digestive enzymes to neutralize the acidic chyme and break down the nutrients for absorption. Pancreatic enzymes are specialized according to each macronutrient and can digest approximately half of all ingested carbohydrates, half of all proteins, and almost all (80–90%) of ingested fat.16
Protein peptides are hydrolyzed into amino acids by a group of protein-based enzymes called proteases that include trypsinogen, chymotrypsinogen, procarboxypeptidase, proelastase, and collagenase.16 Proteases are formed in the pancreas and must travel to the small intestine to complete digestion before they are absorbed.
Fat droplets are first hydrolyzed by bile salts before pancreatic enzymes complete the process. Bile salts are composed of bile, an alkaline solution made and secreted liver that mixes with electrolytes, pigments, and other substances to emulsify fat.16 This step allows pancreatic lipases made in the pancreas to completely digest fat for absorption.
Digestion and absorption of disaccharides greatly depend on the availability of enzymes within the small intestine. Disaccharides first move into the duodenum and jejunum where lactase, sucrase, and maltase act upon each of their constituents. Lactase cleaves a lactose molecule to yield one galactose and one glucose, sucrase hydrolyzes sucrose to yield one glucose and one fructose residue, and maltase hydrolyzes maltose to yield two glucose units. Once they reach the ileum, pancreatic amylase completes the final digestion before monosaccharides are absorbed.
Transport
Following absorption of the smaller constituents by the villi of the ileum, water-soluble nutrients such as amino acids and monosaccharides, water-soluble vitamins, and electrolytes move across the intestinal mucosa into the portal blood until reaching the liver. The products of fat digestion such as monoacylglycerols and long-chain fatty acids must become reesterified to water-soluble molecules before crossing the intestinal barrier. Fatty acids reform to TAGs and combine with cholesterol and phospholipids to form chylomicrons.
Chylomicrons consist of a lipid core made of hydrophobic chains of fat, and a shell made of phospholipid heads that can move through water.16 Unlike water-soluble nutrients, fat-soluble nutrients travel from lymphatic vessels into blood vessels and directly into the heart without making a first pass through the liver.
Excretion
The undigested material that has not been absorbed in the small intestine must move out from the ileum into the large intestine. The primary functions of the colon are (1) absorption of water and electrolytes from the ingesta, (2) microbial fermentation of undigested polysaccharides and resistant protein, and (3) formation and storage of feces.16 The formation of stool or feces begins with mixing neutralized chyme with mucus. Organic materials that the body can’t further process are digested and fermented by bacteria in the colon, and the remaining water left is absorbed. Normal feces are roughly 70% to 75% water and 20% to 25% solids.16
Metabolism
Metabolism is the sum of chemical reactions, secretions, and changes that occur within cells of organ tissues to provide vital energy for the body.16 The metabolic processes involved in the body include anabolic and catabolic pathways. Anabolism or anabolic reactions are the metabolic processes that involve the synthesis of macromolecules such as proteins, glycogen, various lipids, and nucleic acids which promote growth. Catabolism or catabolic reactions are the metabolic processes involved in the breakdown of organic compounds to CO2 and H2O with the release and breakdown of energy. The three organ systems that metabolize nutrients for storage and energy are the liver, the skeletal muscle, the adipose tissue, and the brain.16
Carbohydrates
The metabolic fate of monosaccharides depends on the body’s energy needs. In the fed state, glucose levels start to rise and signal insulin in the pancreas to absorb glucose into the cells. Under these conditions, most tissues (liver, skeletal muscle, adipose, brain, and red blood cells) will increase glucose uptake, oxidation of glucose into energy, and storage for later use.17
The main catabolic pathways that take place in the fed state are glycolysis, tricarboxylic acid (TCA) cycle or citric acid cycle, and the pentose phosphate pathway (PPP).17
Glycolysis is the pathway that breaks down glucose into pyruvate.17 Glycolysis has two fates depending on the availability of oxygen. When oxygen is present (aerobic glycolysis), glucose makes pyruvate enter the mitochondria and be oxidized to acetyl-CoA, which will enter the TCA cycle.17 When oxygen is limited or energy demands exceed oxygen supply, the cell relies on anaerobic glycolysis.
In this case, lactate or lactic acid is formed, but the energy produced through this process is much less than through aerobic oxidation and therefore less favorable.17 If lactic acid levels start to rise, the Cori cycle takes place, by releasing lactate from the tissue, transporting it to the liver, and converting it back to pyruvate.17
The TCA cycle, also known as the citric acid cycle or Krebs’s cycle, is the pathway that takes place in the mitochondria to convert pyruvate into energy.16 This can only take place in the presence of oxygen and acetyl-CoA, an intermediate breakdown product of carbohydrates, protein, and fat. This cycle produces 90% of the body’s energy as ATP and results information of carbon dioxide (CO2) and water (H2O).17
Monosaccharides can also undergo anabolic pathways in the fed state. The most important pathway is glycogenesis. This process synthesizes single units of glucose into glycogen to serve as the main storage form of carbohydrates in the liver and skeletal muscle.17 On the contrary, when the body is in the fasted state, it will decrease serum glucose levels by the actions of glucagon in the pancreas and utilize alternative fuels for energy.17Glycogenolysis is the catabolic pathway that takes place in the fed state and forms glucose from glycogen stores to maintain blood glucose levels.17
Fat
The adipose tissue is the main site for fat metabolism and storage. In the fed state, glucose, as well as dietary fat and cholesterol (transported as chylomicrons), are taken up by the adipose tissue.17 Dietary fat undergoes lipogenesis, an anabolic reaction that oxidizes glucose to glycerol and synthesizes them to triacylglycerols (TAGs).17
The liver can also synthesize fat but should never store fat. To prevent fat accumulation, the liver is equipped with lipotropic factors that promote the removal of fat from the liver].16 During a fasting state, the signaling of hormones such as glucagon and growth hormone will stimulate the activation of lipolysis.17 Lipolysis is a catabolic pathway that releases fatty acids from stored triacylglycerols and provides an oxidizable substrate for the skeletal muscle and liver.17
Protein
Protein metabolism mainly takes place in the liver. Since protein can’t be stored in the body, once protein needs are met, any protein excess is used to make fat and fat storage deposits, and energy, or is removed by the kidneys in the urine.
In the fed state, protein synthesis is the main anabolic reaction that takes place in the ribosomes of liver cells to form proteins from amino acids.17 This pathway involves a complex interplay of many macromolecules including ribosomes, messenger RNA (mRNA), transfer RNA (tRNA), the genetic code, and protein factors.16
Muscle protein synthesis (MPS) is the metabolic process that describes the incorporation of amino acids into bound skeletal muscle proteins.18 Muscle proteins can be classified into contractile myofibrillar proteins (i.e., myosin, actin, tropomyosin, troponin) and energy-producing mitochondrial proteins.18
Depending on diet and translation needs, excess amino acids will undergo amino acid catabolism where amino acids split off the nitrogen groups to form free ammonia. Given that ammonia in the blood can be toxic, it must be converted into urea through the urea cycle, to safely remove it from the blood and into the kidneys.17 Some of it can be converted into purines, and some are used to make the nonessential amino acids through transamination. Excess amino acids are not stored, rather the deaminated carbon skeletons can be stored as glycogen or fat.17
In the fasted state, the main anabolic pathways that take place are gluconeogenesis and ketogenesis in the liver. Gluconeogenesis is an anabolic process that synthesizes glucose from lactate, amino acids, or glycerol. The glucose produced is released into the bloodstream to maintain blood glucose and provide energy for the brain and red blood cells (RBC).17
Ketogenesis is the biochemical process through which organisms produce ketone bodies by breaking down mostly ketogenic amino acids and fatty acids to serve as energy supply for certain organs, particularly the brain, heart, and skeletal muscle.17 Ketogenesis and gluconeogenesis are similar in that they are both chemical processes that provide energy to the body when not enough carbohydrate is present in the diet. However, ketogenesis differs in that it produces ketones to be used as fuel, rather than glucose.17
Macronutrient Content in Foods
Carbohydrates
Carbohydrate is an umbrella term that encompasses sugar, fruits, vegetables, fibers, and legumes. Complex carbohydrates (oligosaccharides or polysaccharides) are generally preferred over simple carbohydrates because they take longer to digest and have a more gradual effect on the increase in blood sugar, whereas simple carbohydrates (monosaccharides) can rapidly raise blood glucose levels upon digestion. In some cases quick digesting carbohydrates are needed, but in most scenarios, slower carbohydrates are preferable, due to longer levels of energy.
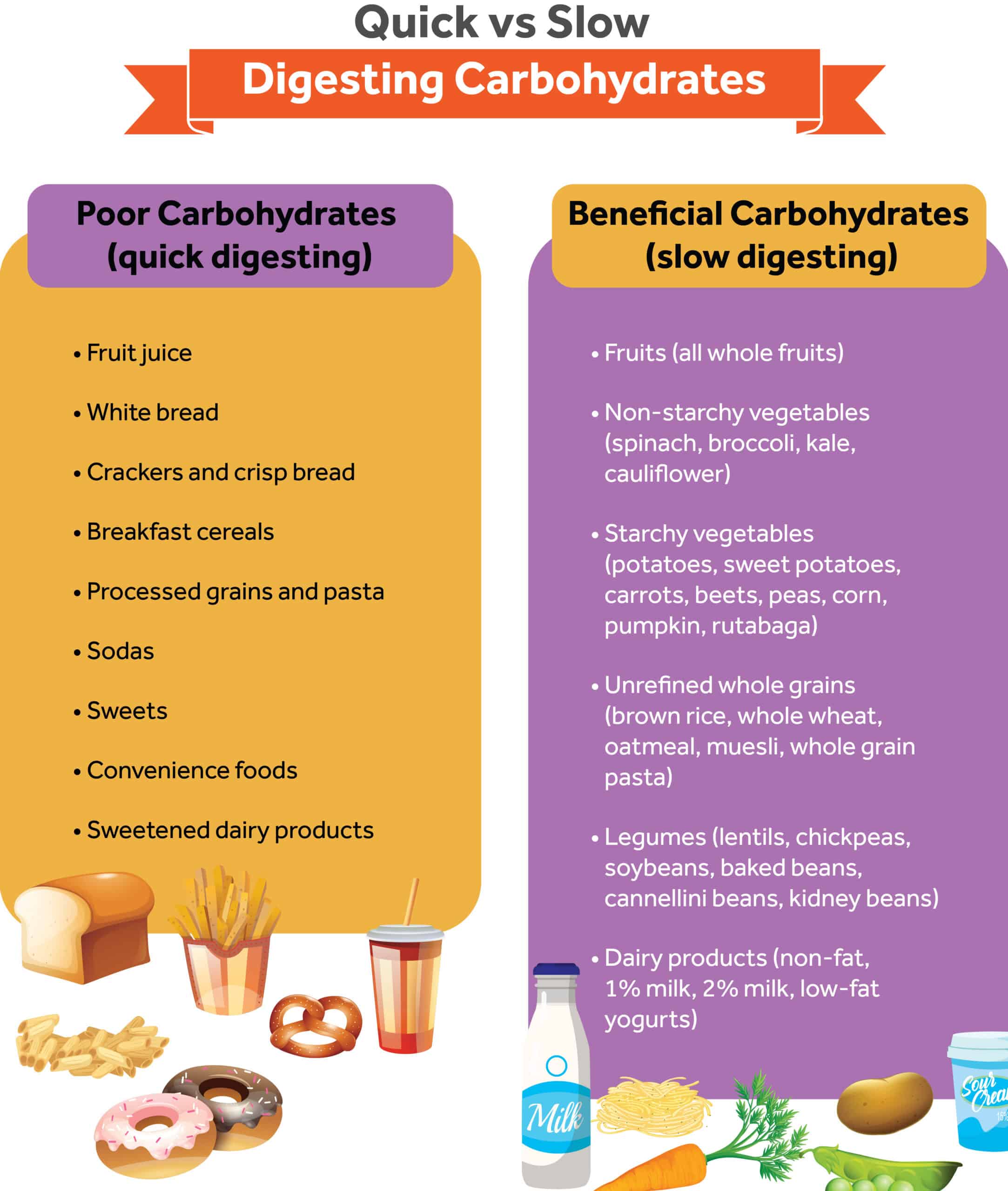
The individual effects of food on blood sugar can be measured by the glycemic index scale that ranks carbohydrates from 0 to 100 based on how rapidly the rise in blood glucose occurs upon consumption.19 The following lists food items as poor or beneficial sources of carbohydrates in terms of slow digestion.
Poor carbohydrates (quick digesting)
- Fruit juice
- White bread
- Crackers and crisp bread
- Breakfast cereals
- Processed grains and pasta
- Sodas
- Sweets
- Convenience foods
- Sweetened dairy products
Beneficial carbohydrates (slow digesting)
- Fruits (all whole fruits)
- Non-starchy vegetables (spinach, broccoli, kale, cauliflower)
- Starchy vegetables (potatoes, sweet potatoes, carrots, beets, peas, corn, pumpkin, rutabaga)
- Unrefined whole grains (brown rice, whole wheat, oatmeal, muesli, whole grain pasta)
- Legumes ( lentils, chickpeas, soybeans, baked beans, cannellini beans, kidney beans)
- Dairy products (non-fat, 1% milk, 2% milk, low-fat yogurts)
Protein
Complete protein sources are generally of animal origin except for some plant-based foods. Complete protein refers to foods that contain all the essential amino acids required in the diet.20 Despite this, it would be wrong to assume that animal-based foods provide more protein than plant-based ones.20 Not all plant foods are low in the same amino acids, so eating a variety of plant-based foods can provide all nine of the essentials.20 Complete animal proteins include eggs, dairy, meat, and seafood; whereas complete plant-based foods mainly include soy. Other plant-based proteins are likely deficient in one or more of the essential amino acids.
High protein foods
- Meat (7g protein/oz)
- Fish and shellfish (7g protein/oz)
- Eggs (7g protein/oz)
- Cow’s Milk (8g protein/cup)
- Goat’s Milk (9g protein/cup)
- Soy Milk (7-8 g protein/cup)
- Plain yogurt (6-7g protein/1/2 cup)
- Greek yogurt: (11-15g protein/1/2 cup)
- Cheese (7g protein/1oz)
- Nut butter (8g protein/2 Tbsp)
- Tofu (4.6 g protein/oz)
- Lentils, cooked (10g protein/1/2 cup)
- Chickpeas, cooked (8g protein/1/2 cup)
- Quinoa, cooked (4g protein/1/2 cup)
- Teff, cooked (5g protein/1/2 cup)
- Chia seeds (5g protein/oz)
Fats
Fats and oils are naturally found in both plants and animal foods, and, most recently, commercially prepared as hydrogenated oils. Oils are classified by their stability at room temperature and essentiality. Particularly trans fats, saturated fats, and some omega-6 vegetable oils have been shown to promote inflammation, whereas a diet high in monounsaturated fat and essential omega-3 fats have been shown to inhibit and reduce inflammation by interfering with pro-inflammatory compounds naturally made by the body.13, 14 Diets supplemented with omega-3 fats have been shown to reduce post-exercise delayed-onset muscle soreness and inflammation and promote healing.21
Essential Fats
- Seeds
- Nuts
- Legumes
- Fish and shellfish
- Vegetable oils
Non-Essential Fats
- Tropical oils
- Vegetable oils
- Peanut oil
- Butters and solid fats
- Red meats
- Dairy products
- Snacks
Macronutrient Recommendations for Fitness Goals
Dietary Intake Guides
The Recommended Dietary Allowance (RDA), first established in 1941 by the Food and Nutrition Board of the Institute of Medicine, defined the average daily amount of nutrients to meet the needs of most healthy people.5 With changes to the food supply and needs of the general population, the RDAs were adapted into a framework of nutrient recommendations called dietary reference intakes (DRIs). Included in the DRIs are RDAs, as well as guidance on safe upper limits (ULs) of vitamins and minerals.
The Dietary Guidelines for Americans (DGAs) are evidence-based guidelines revised and published every five years by the National Academy of Sciences Food and Nutrition Board of the Institute of Medicine (IOM) in conjunction with the U.S. Department of Agriculture.22 The first ever published guidelines were a federal government response to the increasing national concern for the rise in nutrition-related chronic diseases.19
Today, the DGAs are used by accredited nutrition professionals to assist the public in consuming a healthy diet.22 For other health and community professionals, including the government, the information in the DGA can be incorporated into community programs and used to create educational materials for consumers and health initiatives.22
In 2011 the MyPlate guidelines from the USDA replaced the previous MyPyramid diagram.23 The MyPlate is designed for the general population and serves as a food guidance system to choose foods from within and across food groups to meet nutrient needs.23 The amounts vary based on a person’s gender and age.
Generally, MyPlate suggests that adults consume the following each day: at least 2 cups of fruits, 2 and 1⁄2 cups of vegetables, a minimum of 3 oz of whole grains, at least 1 and 1⁄2 cups of beans and peas weekly, 5 to 6.5 oz of protein, and 3 cups of dairy.
Macronutrient Requirements
Carbohydrates
According to the RDAs, healthy adult diets should consume 130 grams of carbohydrates per day to maintain the most essential functionalities of the brain.5 The Acceptable Macronutrient Distribution Range (AMDR) suggests including 45 to 65% of daily calories in the form of carbohydrates, or 225 and 325 grams of carbohydrates based on a daily 2,000 calorie diet.5
Recommendations for daily carbohydrate intake in the athlete population vary by gender, age, body mass, and training needs. A carbohydrate intake of 5 to 7 g/kg/day can meet the general training requirements, an intake of 7 to 10 g/kg/day of carbohydrates will likely suffice for endurance athletes, and for elite athletes training 5 to 6 hours a day, 12 g/kg/day or a range of 420 to 720 g of carbohydrates are appropriate.24
Carbohydrate intake will also vary greatly depending on the training modality. When glycogen stores drop to critically low levels, the athlete must either stop exercising or drastically reduce the pace. If athletes experience glycogen depletion after exercise, a carbohydrate intake of 1.5 g/kg body weight during the first 30 minutes and again every 2 hours for 4 to 6 hours is recommended.19
As a general recommendation, athletes should consume a mixed meal after strenuous training that provides a balance of all three macronutrients to help build and repair muscle tissue. If the goal of the client is solely to gain a healthy weight of lean muscle tissue, an additional 500 to 1,000 calories per day can be added in addition to strength training.19
Protein
Protein requirements greatly vary depending on the age, body size, and physiological state, as well as the level of energy intake of each individual. The RDA of protein for adults (men and women aged 19 years and older) is set at 0.8 grams of protein per kilogram of body weight to maintain basic function.5 The AMDR for protein is 10 to 35% of calories for adults or about 50 to 175 grams per day for people consuming 2,000 calories per day.5
The athletic population will have an increased need for protein intake depending on the training modality that the individual is engaged in. For endurance athletes, nitrogen balance studies in men suggest a protein recommendation of 1.2g/kg per day.25
If resistance training is the main modality, protein requirements are higher than endurance exercise, and it has been recommended that experienced male bodybuilders and strength athletes consume 1.6 to 1.7g/kg/day to allow for the accumulation and maintenance of lean tissue.26, 27 For athletes interested in muscle hypertrophy, it appears that neither the type nor the number of proteins matters if the day’s total amount is within the recommended range for resistance-training athletes of 1.2 to 2 g/kg/day.19
Protein intake after training is essential to help build and repair muscle tissue. Research shows that a minimum of 30 g of high-quality protein at each meal that contains 2.5 g leucine per meal optimally stimulates protein synthesis, and when leucine and omega-3 fatty acid are supplemented there is a reduction in muscle loss for acutely injured athletes.21
Fats
The Food and Nutrition Board of the IOM has not established RDAs for fats.5 The AMDR for fat is between 20 to 35% of total dietary calories for adults age 19 and older or about 44 to 77 grams of fat per day if consuming a 2,000-calorie diet.5 The AMDRs recommend adjusting the number of calories coming from fat based on the type of fat. It is recommended that monounsaturated fats represent 15% to 20% of total calories/day, polyunsaturated fat 5% to 10% of total calories/day, saturated fat less than 10% of total calories/day, cholesterol less than 300 mg/day, and completely zero trans fats.5 The IOM also gives recommendations for the two essential fatty acids: linoleic acid (men, 14–17 g/d; women, 11-I2g/d) and linolenic acid (men, 1.6 g/d; women, I. I g/d).5
Fat is a macronutrient that should never be disregarded in the dietary pattern of athletes, since there is no performance difference with less than 15% of energy from fat, compared with 20% to 25% of energy from fat].28 Fat is also essential in athletes’ dietary intake as it provides energy, fat-soluble vitamins, and essential fatty acids.
Hydration Requirements and Strategies
Water Function
Water (H2O) is an essential nutrient that makes up the largest component of the body, accounting for about 73% of lean body mass in adults.19 As a vital nutrient to both humans and plants, water functions to (1) dissolve nutrients, minerals, gasses, and enzymes, (2) regulate body temperature, (3) lubricate and moisten tissues, (3) transport nutrients and oxygen into cells and remove excess waste, (4) maintain blood volume and acid-base (pH) balance.19
Electrolytes
Within fluid systems in the body exist electrolytes, and electrically charged minerals that regulate fluid balance, movement, and distribution within other compartments. Electrolytes are responsible for (1) the maintenance of physiologic body functions, (2) cellular metabolism, (3) neuromuscular function, and (4) osmotic equilibrium.19 The major extracellular electrolytes are sodium (Na+), calcium (Ca2+), chloride (Cl-), and bicarbonate (HCO3-). Potassium (K+), magnesium (Mg2+)., and phosphate (PO ₄)³⁻ .19
Dehydration
Water is naturally lost throughout the day by the respiratory tract, skin, gastrointestinal tract, and kidneys. During physical exercise, the body increases the rate of sweat production leading to substantial water and electrolyte losses. If sweat water and electrolyte losses are not replaced then the individual will dehydrate during physical activity.
Dehydration refers to the loss of body water of 2% or more of body weight.19 The typical symptoms of dehydration include extreme thirst, decreased urine output, secretion of concentrated urine, headaches, fatigue, muscle cramps, hypotension, and fever.19
The effects of body water loss ultimately alter the functionalities of the central nervous system, thermoregulatory system, cardiovascular system, and metabolic functions. Excessive dehydration can increase the risk for heat exhaustion29, 30, 31 and heat stroke32, 33, 34, 35 In addition, dehydration has been associated with reduced autonomic cardiac stability36 altered intracranial volume,37 and reduced cerebral blood flow velocity responses to orthostatic challenges.38
Water and Electrolyte Requirements
For an individual to maintain a water balance, the amount of water consumed must equal the amount lost from the body. The body can maintain a water balance by releasing and regulating hormones including antidiuretic hormone, aldosterone, angiotensin II, cortisone, norepinephrine, and epinephrine.39 The minimal amount of daily water to replace obligatory water losses from the respiratory tract, skin, feces, and urine is about 1.44 L. Calculations of daily water intake are also based on age group and exercise intensity.
Adults
According to the IOM, the general fluid requirements for adults are based on the formula 35 m/kg or 1mL/kcal of energy expenditure.40 The IOM also recommends adequate intake (AI) values for total water at levels to prevent dehydration.40 The AI for men aged 19+ is 3.7 liters each day, and 3 liters (13 cups) of which should be consumed as beverages.40 The AI for women aged 19+ is 2.7 liters about 2.2 liters (9 cups) which should be consumed as beverages each day.40
Special attention must be given to this population given their increased risk for dehydration. The EFSA reviewed the literature and recommended an Adequate Intake (AI) of 2.0 L/day for women and 2.5 L/day for men of all ages (from a combination of drinking water, beverages, and food).41 Pregnancy and Lactation Pregnancy is also at risk for dehydration given the increased needs of the fetus, and the amniotic fluid. The water requirements for pregnant women are the same as in non-pregnant women plus an increase in proportion to the increase in energy intake (300 mL/day) is proposed. For lactating women, adequate water intakes of about 700 mL/day above the AIs of non-lactating women of the same age are derived.
Physical Activity
The level of physical activity of adults can also impact water requirements. The following guidelines can be used to assess fluid requirements before, during, and after physical activity:
Before an activity it is recommended to drink 17 to 20 oz of water 2 to 3 hours before the start of exercise or during warm-up to maintain normal plasma electrolyte levels.40 Consumption of sodium in beverages (20-50 mEq/L) and/or small amounts of salted snacks or sodium-containing foods at meals helps to stimulate thirst and retain the consumed fluids.40 On the contrary, hyperhydration can lower plasma sodium and increase the risk of dilutional hyponatremia.40
During activity it is suggested to drink 7-10 ounces of fluid every 10 to 20 minutes to prevent excessive dehydration.40 Dehydration results in a decrease in blood volume and an increase in heart rate. In prolonged exercise lasting greater than 3 hours, such as for marathon runners, a possible starting point is to drink ad libitum from 0.4 to 0.8 L/hr.40
Restoring hydration can be accomplished by drinking around 1.5 L/kg of body weight loss.40 When possible, it is recommended that fluids are consumed over time (and with sufficient electrolytes) rather than being ingested in large boluses to maximize fluid retention .42, 43
Water replacement in the absence of supplemental sodium can lead to decreased plasma sodium concentrations.19 When plasma sodium levels fall below 130 mEq/L, the individual can experience lethargy, confusion, seizures, or loss of consciousness.40 Exercise-induced hyponatremia may result from fluid overloading during prolonged exercise over 4 hours.40
Hyponatremia is associated with individuals who drink plain water above their sweat losses or who are less physically conditioned and produce a saltier sweat.40 Another important electrolyte, potassium, can decrease through sweat, but the loss of 32 to 48 mEq/day does not appear to be significant and is easily replaced by diet.40
Hot Weather Conditions
For individuals performing prolonged physical activity in hot weather, drinking fluid replacements or also known as electrolyte replacement is suggested. Beverages containing approximately 20-30 mEq/L of sodium (chloride as the anion), 2-5 mEq/L of potassium, and 5-10% carbohydrate are recommended.44 The sodium and potassium are to help replace sweat electrolyte losses, while sodium also helps to stimulate thirst, and carbohydrate provides energy.44 These components also can be consumed by nonfluid sources such as gels, energy bars, and other foods.44
Summary
Macronutrients provide the essential energy for growth, maintenance, metabolic functions, and survival. Healthy adults should consume adequate amounts of protein, carbohydrates, and fat based on their weight and calorie requirements. Water is a vital nutrient that dissolves nutrients, regulates temperature, lubricates tissues, transports important products across cells and removes excess waste, along with maintaining blood volume and acid-base balance in the body. Water and electrolytes are lost throughout the day and must be replenished, especially with added activity or warm weather conditions.
References
- Harper, A. E. Defining the essentiality of nutrients. In M. E. Shils, J. A. Olson, M. Shike, & A. C. Ross (Eds.), Modern nutrition in health and disease (9th ed, pp. 3–10). Baltimore: Williams & Wilkins. 1999.
- Rudman D, Feller A. Evidence for deficiencies of conditionally essential nutrients during total parenteral nutrition. J Am Coll Nutr. 1986;5(2):101-106. https://doi.org/10.1080/07315724.1986.10720117
- Beman, J. Energy Economics in Ecosystems. 2010. Nature Education Knowledge 3(10):13
- National Research Council (US) Committee on Diet and Health. Diet and Health: Implications for Reducing Chronic Disease Risk. Washington (DC): National Academies Press (US); 1989.
- Trumbo P, Schlicker S, Yates AA, Poos M; Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. J Am Diet Assoc. 2002;102(11):1621-1630. https://doi.org/10.1016/s0002-8223(02)90346-9
- Madigan MT, Brock TD, Parker J, Martinko JM. Brock Biology of Microorganisms: International Edition. 10th ed. Pearson; 2002.
- Murray RK, Bender D, Botham KM, Kennelly PJ, Rodwell VW, Weil PA. Harper’s Illustrated Biochemistry. 29th ed. McGraw-Hill Medical; 2012.
- Nelson DL, Cox MM. Lehninger Principles of Biochemistry. 8th ed. W. H. Freeman; 2021.
- Swagerty DL Jr, Walling AD, Klein RM. Lactose intolerance [published correction appears in Am Fam Physician. 2003 Mar 15;67(6):1195]. Am Fam Physician. 2002;65(9):1845-1850.
- Garrett RH, Grisham CM. Biochemistry. 4th ed. Brooks/Cole; 2010.
- Rose, W. C. Feeding experiments with mixtures of highly purified amino acids: I. The inadequacy of diets containing nineteen amino acids. The Journal of Biological Chemistry. 1931; 94, 155–165.
- de Roos NM, Schouten EG, Katan MB. Trans fatty acids, HDL cholesterol, and cardiovascular disease. Effects of dietary changes on vascular reactivity. Eur J Med Res. 2003;8(8):355-357.
- Massaro M, Scoditti E, Carluccio MA, Montinari MR, De Caterina R. Omega-3 fatty acids, inflammation, and angiogenesis: nutrigenomic effects as an explanation for anti-atherogenic and anti-inflammatory effects of fish and fish oils. J Nutrigenet Nutrigenomics. 2008;1(1-2):4-23.
- Wall R, Ross RP, Fitzgerald GF, Stanton C. Fatty acids from fish: the anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr Rev. 2010;68(5):280-289. https://doi.org/10.1111/j.1753-4887.2010.00287.x
- Blesso CN, Fernandez ML. Dietary Cholesterol, Serum Lipids, and Heart Disease: Are Eggs Working for or Against You?. Nutrients. 2018;10(4):426. Published 2018 Mar 29. https://doi.org/10.3390/nu10040426
- Stipanuk, M. H. Biochemical, physiological, & molecular aspects of human nutrition. 3rd ed. St. Louis: Saunders Elsevier; 2006.
- Lieberman, M., A. and Peet, eds. Marks’ Basic Medical Biochemistry: A Clinical Approach. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2018, Chapter 2: The Fed or Absorptive State, Chapter 3: The Fasted State.
- Witard OC, Bannock L, Tipton KD. Making Sense of Muscle Protein Synthesis: A Focus on Muscle Growth During Resistance Training. Int J Sport Nutr Exerc Metab. 2022;32(1):49-61. https://doi.org/10.1123/ijsnem.2021-0139
- Mahan LK, Escott-Stump S. Krause’s Food, Nutrition, and Diet Therapy. 11th ed. W B Saunders; 2003.
- Smith J, Gropper S, Carr T. Advanced Nutrition and Human Metabolism. 8th ed. Wadsworth Publishing; 2021
- Tipton KD. Dietary strategies to attenuate muscle loss during recovery from injury. Nestle Nutr Inst Workshop Ser. 2013;75:51-61. https://doi.org/10.1159/000345818
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans, 2020-2025. 2020. 9th Edition. https://www.dietaryguidelines.gov/
- U.S. Department of Agriculture. MyPlate. 201. http://www.choosemyplate.gov/
- Driskell JA, Wolinsky I, eds. Nutritional Assessment of Athletes, Second Edition. CRC Press; 2016. https://doi.org/10.1201/b10203
- Fraser CL, Kucharczyk J, Arieff AI, Rollin C, Sarnacki P, Norman D. Sex differences result in increased morbidity from hyponatremia in female rats. Am J Physiol. 1989;256(4 Pt 2):R880-R885. https:/doi.org/10.1152/ajpregu.1989.256.4.R880
- Fraser CL, Arieff AI. Epidemiology, pathophysiology, and management of hyponatremic encephalopathy. Am J Med. 1997;102(1):67-77. https://doi.org/10.1016/s0002-9343(96)00274-4
- Fraser CL, Sarnacki P. Na+-K+-ATPase pump function in rat brain synaptosomes is different in males and females. Am J Physiol. 1989;257(2 Pt 1): E284-E289. https://doi.org/10.1152/ajpendo.1989.257.2.E284
- Rodriguez NR, DiMarco NM, Langley S; American Dietetic Association; Dietitians of Canada; American College of Sports Medicine: Nutrition and Athletic Performance. Position of the American Dietetic Association, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and athletic performance. J Am Diet Assoc. 2009;109(3):509-527. https://doi.org/10.1016/j.jada.2009.01.005
- Adolph E.F. and associates. Physiology of Man in the Desert. 1970. Am J Trop Med Hyg;19(3):576-576. https://doi.org/10.4269/ajtmh.1970.19.3.tm0190030576a
- McLellan TM, Cheung SS, Latzka WA, et al. Effects of dehydration, hypohydration, and hyperhydration on tolerance during uncompensable heat stress. Can J Appl Physiol. 1999;24(4):349-361. https://doi.org/10.1139/h99-027
- Sawka MN, Young AJ, Latzka WA, Neufer PD, Quigley MD, Pandolf KB. Human tolerance to heat strain during exercise: influence of hydration. J Appl Physiol (1985). 1992;73(1):368-375. https://doi.org/10.1152/jappl.1992.73.1.368
- Carter R 3rd, Cheuvront SN, Williams JO, et al. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc. 2005;37(8):1338-1344. https://doi.org/10.1249/01.mss.0000174895.19639.ed.
- Epstein Y, Moran DS, Shapiro Y, Sohar E, Shemer J. Exertional heat stroke: a case series. Med Sci Sports Exerc. 1999;31(2):224-228. https://doi.org/10.1097/00005768-199902000-00004
- Centers for Disease Control (CDC). Exertional rhabdomyolysis and acute renal impairment–New York City and Massachusetts, 1988. MMWR Morb Mortal Wkly Rep. 1990;39(42):751-756.
- Centers for Disease Control and Prevention (CDC). Hyperthermia and dehydration-related deaths associated with intentional rapid weight loss in three collegiate wrestlers–North Carolina, Wisconsin, and Michigan, November-December 1997. MMWR Morb Mortal Wkly Rep. 1998;47(6):105-108.
- Carter R III, Cheuvront SN, Wray DW, Kolka MA, Stephenson LA, Sawka MN. The influence of hydration status on heart rate variability after exercise heat stress. J Therm Biol. 2005;30(7):495-502. https://doi.org/10.1016/j.jtherbio.2005.05.006
- Strachan A, Watson P. The effects of dehydration on brain volume–preliminary results. Int J Sports Med. 2006;27(4):342. doi:10.1055/s-2006-924007
- Carter R 3rd, Cheuvront SN, Vernieuw CR, Sawka MN. Hypohydration and prior heat stress exacerbates decreases in cerebral blood flow velocity during standing. J Appl Physiol (1985). 2006;101(6):1744-1750. https://doi.org/10.1152/japplphysiol.00200.2006
- Kingley J: Fluid and electrolyte management in parenteral nutrition, Support Line 27:13, 2005.
- American College of Sports Medicine, Sawka MN, Burke LM, et al. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc. 2007;39(2):377-390. https://doi.org/10.1249/mss.0b013e31802ca597
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific opinion on dietary reference values for energy. 2013. EFSA J. 11, 3005.
- Kovacs EM, Schmahl RM, Senden JM, Brouns F. Effect of high and low rates of fluid intake on post-exercise rehydration. Int J Sport Nutr Exerc Metab. 2002;12(1):14-23. https://doi.org/10.1123/ijsnem.12.1.14
- Wong SH, Williams C, Simpson M, Ogaki T. Influence of fluid intake pattern on short-term recovery from prolonged, submaximal running and subsequent exercise capacity. J Sports Sci. 1998;16(2):143-152. https://doi.org/10.1080/026404198366858
- Institute of Medicine (US) Committee on Military Nutrition Research, Marriott BM, eds. Fluid Replacement and Heat Stress. Washington (DC): National Academies Press (US); 1994.