Micronutrients are the compounds necessary to maintain the daily functions of the human body. These encompass organic and inorganic compounds such as vitamins and minerals.1 There are nearly 30 of these nutrients considered to be essential because the body cannot manufacture them in sufficient amounts. Thus, these micronutrients must be obtained from the diet in small amounts to maintain essential functions in the body, human development, disease prevention, and well-being.1 Given the importance of micronutrients in health and fitness training, fitness professionals should have a working knowledge of the various key micronutrients required in a complete human diet.
Introduction to Micronutrients
Vitamins
Vitamins are organic compounds and are essential nutrients found in plants and animals that are only required in the diet in small amounts to maintain fundamental functions of the body.2 Vitamins are categorized into two groups: water-soluble vitamins (the vitamin B group, C, folic acid, and biotin) and lipid-soluble vitamins (A, D, E, and K).2 The classification of vitamins is based on their solubility, and biochemical and physiological roles in digestion, absorption, and transport rather than chemical structures.3 Another important distinction is that vitamins cannot be transformed into energy to meet metabolic demands nor used for structural purposes but can be easily broken down by heat, acid, or air. Hence vitamins are required in much smaller amounts than carbohydrates, proteins, and fats.3
Minerals
Minerals, or inorganic nutrients, are essential elements found in the soil and water and classified into macro and micro minerals. Macrominerals are composed of calcium, phosphorus, magnesium, sodium, potassium, chloride, and sulfur. The microelements may be considered in two groups: trace elements (iron, zinc, manganese, copper, and fluorine) and ultra-trace elements (selenium, molybdenum, iodine, chromium, boron, and cobalt).3 Other minerals such as arsenic, nickel, vanadium, and silicon have proven some benefits in animal studies but have insufficient evidence to determine their essentiality or benefit for humans.
Role of Micronutrients in the Human Body
Micronutrients play a key role in metabolism, the maintenance of tissue function, and the prevention of critical illness. Optimal intakes of micronutrients are essential to all individuals, with observable clinical benefit in those who are severely depleted. Improper dosing of micronutrients carries its own risks and can be potentially harmful to those who exceed upper limit intakes of vitamins and minerals.4
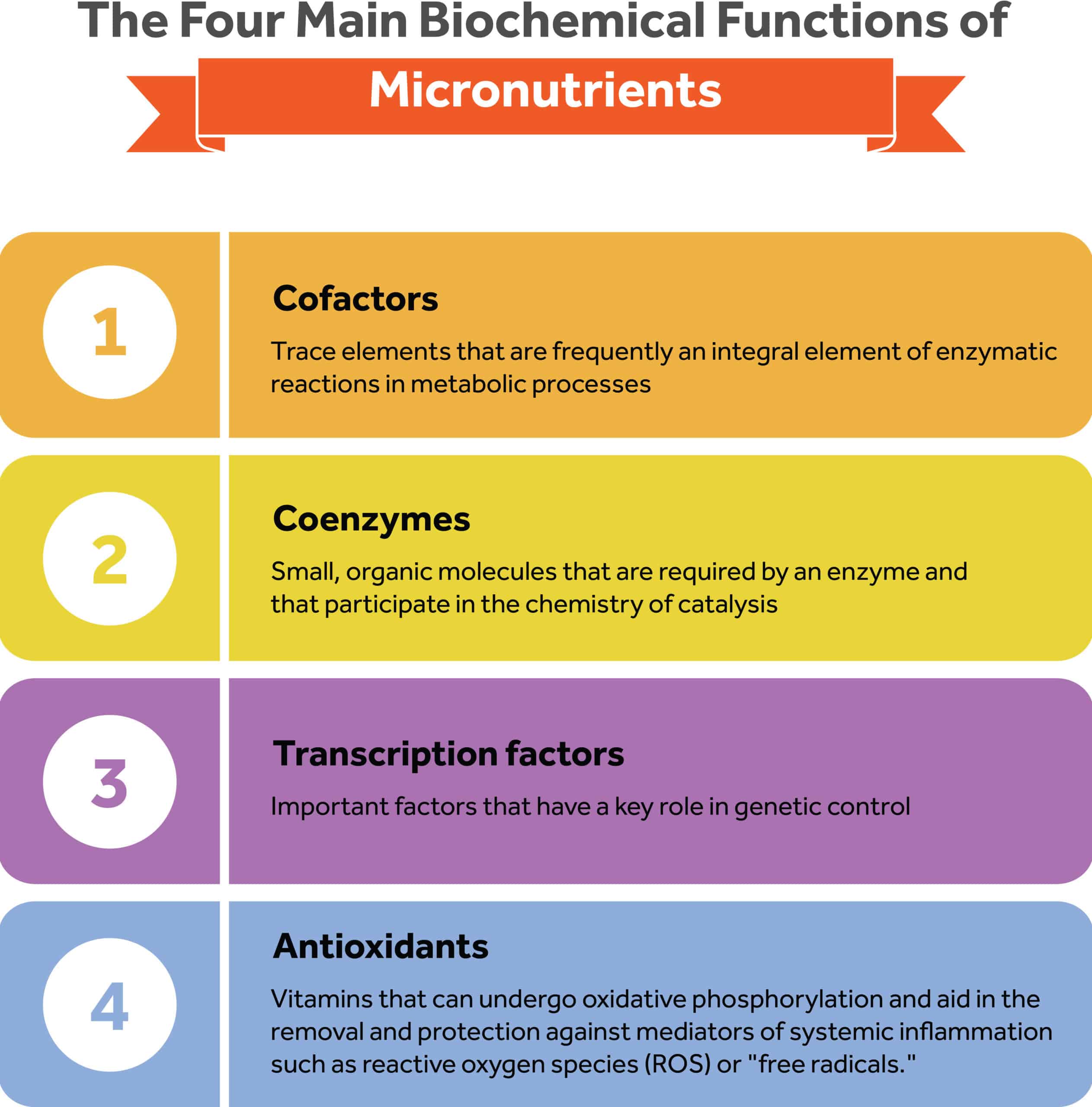
The four main biochemical functions of micronutrients can be summarized below:
- Cofactors: Cofactors are inorganic trace elements whose presence facilitates enzymatic reactions in metabolic processes.4 For example, zinc is a cofactor for over 100 enzymes, whereas selenium is required in the form of selenocysteine within the enzyme glutathione peroxidase.4
- Coenzymes: Coenzymes are defined as small, organic molecules that are required by an enzyme and that participate in the chemistry of catalysis.3 In human biology, coenzymes are the vitamins whose presence is required to facilitate an enzymatic reaction.4 For example, riboflavin and niacin are vitamins that participate in the electron transport chain by acting as intermediary elements to ensure the formation of energy, proteins, and nucleic acids.4
- Transcription factors: Transcription factors are minerals that have a key role in genetic control.4 For example, zinc “fingers” are transcription control factors that bind to DNA and regulate the transcription of receptors for steroid hormones and other factors.4
- Antioxidants: Antioxidants are a class of micronutrients that aid in the removal and protection against mediators of systemic inflammation such as reactive oxygen species (ROS) or “free radicals.”4 Many vitamins have antioxidant properties. For example tocopherol (Vitamin E) is a lipid-soluble antioxidant known to play an important role in scavenging free radicals that damage cells.5 Wound healing and immune function also depend on adequate levels of vitamins and trace elements.6
Vitamins: Functions, Sources, Intake Guidelines, and Deficiencies
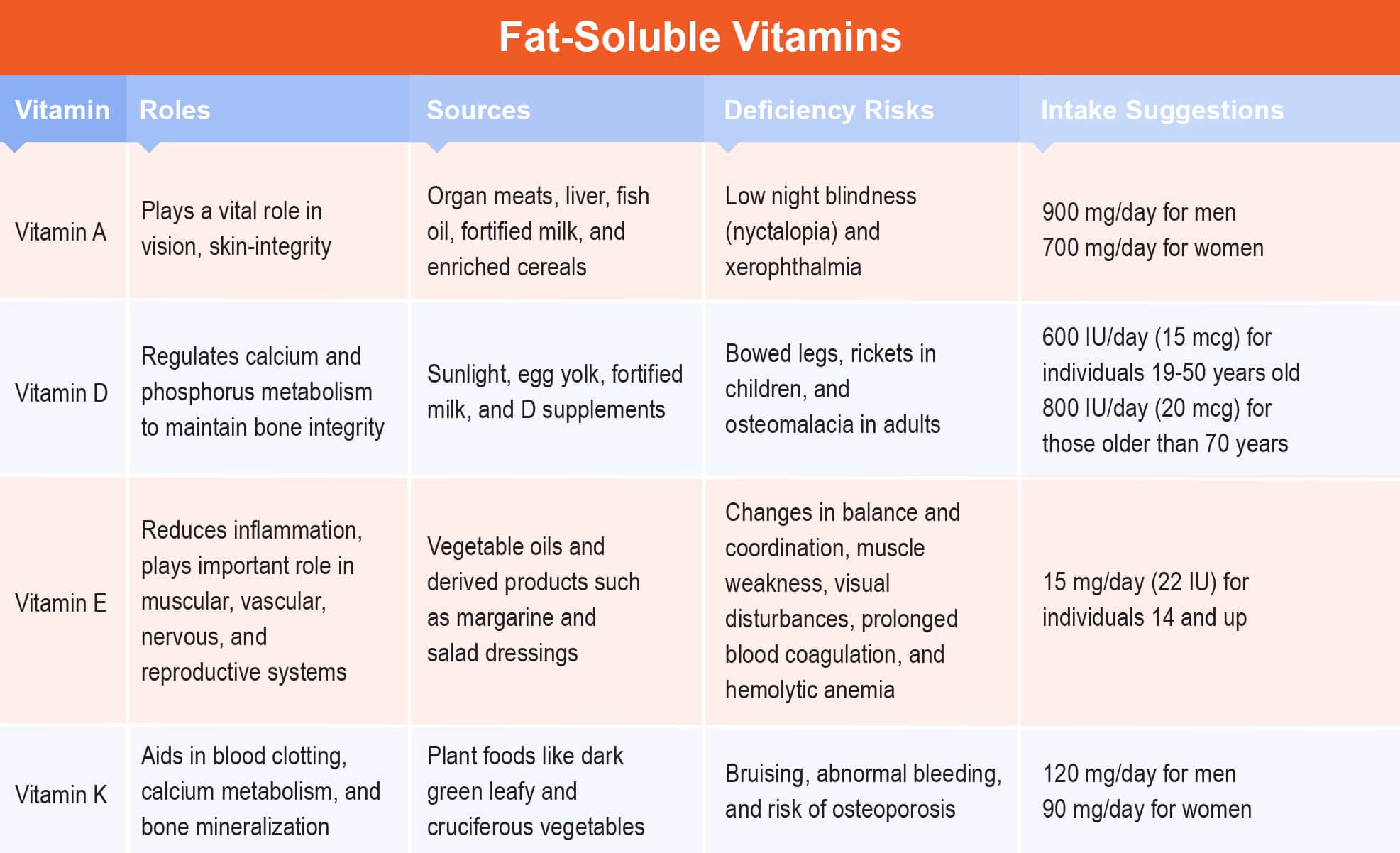
Fat-Soluble Vitamins
Like any other fat, fat-soluble vitamins are absorbed into the lymphatic system before they can travel through the blood in association with protein carriers.7 Fat-soluble vitamins can be stored within the liver or with other lipids in fatty tissues and tend to be susceptible to building up and potentially causing toxicity.7 The requirements for fat solubles vary greatly, but periodic dosages (weeks or even months) are optimal requirements because the body can draw on its stores.7
Vitamin A
Vitamin A (Retinol, Retinoic acid) plays a vital role in vision and skin integrity and is involved in maintaining bone, teeth, nerves, and membrane integrity and functionality.7, 8 The active form of vitamin A is present in organ meats, liver, fish oil, fortified milk, and foods such as enriched cereals. The precursor of vitamin A, beta-carotene, is naturally present in yellow and orange fruits, and dark leafy green vegetables.
When vitamin A supply runs low, night blindness (nyctalopia) can occur.7, 8 This is a reversible process that can be corrected with adequate supplementation. If vitamin A deficiency is not corrected, it can lead to xerophthalmia, a more profound deficiency that results in permanent and irreversible blindness.7, 8
Populations at risk for vitamin A deficiency include those experiencing malnutrition, anorexia nervosa, burns, some forms of cancer, cystic fibrosis, and recent obstructions leading to surgery.7,8
Signs of vitamin A toxicity include headaches, weight loss, abdominal pain, blurred vision, muscle weakness, drowsiness, irritability, and peeling of skin.7, 8 Vitamin A intake that exceeds the tolerable upper limit can lead to congenital birth defects in the eyes, skull, lungs, and heart.7,8 AI for infants is based on the amount of retinol found in human milk. RDA is 900 mg for men and 700 mg for women, adjusted for differences in average body size. UL is 3000 mg/d.9 Vitamin A intake in pregnant women should be restricted if present in supplement form.
Vitamin D
Vitamin D (Calcitriol, D3) regulates calcium and phosphorus metabolism to maintain bone integrity.7, 8 The main sources of vitamin D are sunlight, egg yolks, fortified milk, and supplements, commonly referred to as Vitamin D3 (cholecalciferol).
Plant sources also contain vitamin D in the D2 form (ergocalciferol) and are equally as absorbable as Vitamin D3. The precursor of this fat-soluble vitamin is cholesterol, which must travel to the liver to produce calcidiol, and finally to the kidneys where it becomes metabolically active as calcitriol.7, 8
The prevalence of vitamin D deficiency is especially high in the United States. The 2020-2025 Dietary Guidelines for Americans estimates that more than 90 percent of men and women older than age 19 years do not consume enough vitamin D.9
The most notable signs of vitamin D deficiency are bowed legs, rickets in children, and osteomalacia in adults.7, 8 Susceptible individuals, particularly adolescents, people with dark skin, adult women, housebound elderly people, and many overweight and obese people are at high risk for insufficiency.7, 8 Vitamin D toxicity is rare, however, symptoms such as headache and nausea, upset stomach, bone fragility, and growth retardation have been reported in children receiving doses that exceed the tolerable upper intake.7, 8 The AI for vitamin D recommended is 5-15 ug, UL is 100 mcg (4000 IU)/day, and RDA for individuals 19-50 years old is 600 IU (15 mcg). For those older than 70 years RDA is 800 IU (20 mcg).11
Vitamin E
Vitamin E (Tocopherol, Tocotrienol) acts as a lipid-soluble membrane antioxidant by scavenging free radicals and reducing inflammation.7, 8 Vitamin E has important roles in muscular, vascular, nervous, and reproductive systems and acts as an anticoagulant and vitamin K antagonist.7, 8 Vitamin E is naturally found in vegetable oils and derived products such as margarine and salad dressings, whereas animal fats have virtually none.
Vitamin E deficiency is rare, however, reported symptoms include changes in balance and coordination, muscle weakness, visual disturbances, prolonged blood coagulation, and hemolytic anemia.7, 8
In addition, the toxicity of vitamin E rarely occurs. Excessive doses of vitamin E can lead to dermatitis, fatigue, acne, vasodilation, hypoglycemia, increased requirement for vitamin K, abnormal coagulation and bleeding, and muscle damage.7, 8
Caution should be taken for individuals taking anticoagulant medication, as interactions with coagulant factors can occur and lead to uncontrolled bleeding and unwarranted brain hemorrhages.12
Intake guidelines for vitamin E increase with the use of PUFAs. The RDA for males and females ages 14 years and older is 15 mg/day (22 IU), UL is 1000 mg/day, and AI is 4-12 mg/day based on life stage and gender.9
Vitamin K
Vitamin K’s primary function is to aid in blood clotting, calcium metabolism, and bone mineralization.7, 8 Vitamin K is the only fat-soluble vitamin that is synthesized by bacteria in the gut to form prothrombin, a coagulation factor.7, 8
Vitamin K is mainly found in plant foods like dark green leafy and cruciferous vegetables. Smaller amounts can be found in animal foods such as fish, liver, meat, and eggs.
Vitamin K deficiency can cause bruising and abnormal bleeding due to its critical role in blood clotting.7, 8 Deficiency may also decrease bone density and as a result, increase the risk of osteoporosis.
For individuals taking anticoagulants, vitamin K toxicity can also block the effect of these therapeutic medications.7, 8 However, vitamin K toxicity is rare in healthy populations. Individuals who take large doses of vitamin A or E may also acquire a vitamin K deficiency due to the antagonist roles of the respective vitamins. On the contrary, vitamin K toxicity is rare, but reports have been documented of prolonged bleeding time and breakage of the red blood cells leading to jaundice.7, 8
Instances in which vitamin K is supplemented in doses higher than normal are during pre-surgery, or upon birth to prevent hemorrhagic diseases in newborns. Caution must be adverted to individuals taking anticoagulant medications.7, 8
The RDA and AI are 120 mg/day for men and 90 mg/day for women. No UL has been established, but data is limited and one should not assume that high vitamin K consumption is harmless.9
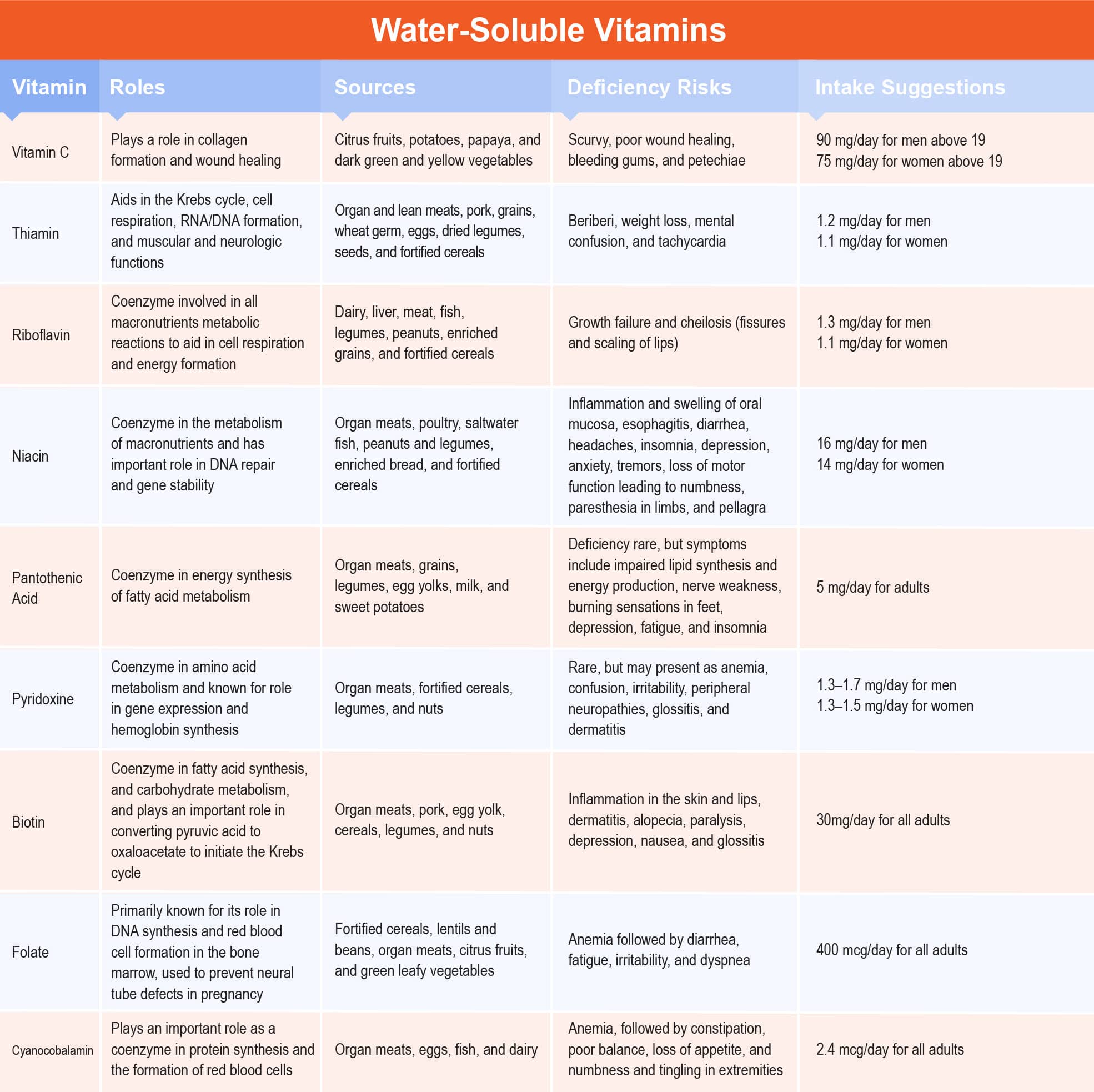
Water-Soluble Vitamins
Different from their constituent fat-soluble vitamins, water-soluble vitamins are absorbed directly into the blood and travel freely in the body through passive diffusion. Water-soluble vitamins cannot be stored, resulting in easy transport through the gut and excretion in the urine.7
Vitamin C
Vitamin C (Ascorbic acid) plays an important role in collagen formation and wound healing, tryptophan to serotonin conversion, folic acid metabolism, and iron absorption.7, 8 Vitamin C can be found in citrus fruits, potatoes, papaya, and dark green and yellow vegetables.
The main signs of vitamin C deficiency are scurvy, poor wound healing, bleeding gums, and petechiae (brown spots on the skin).7, 8 Vitamin C deficiency is especially high in individuals with severe trauma, surgical wounds, burns, cancer, chronic diarrhea, alcoholism, and Alzheimer’s disease.7, 8
Excess vitamin C can occur and often manifests with GI distress and diarrhea.7, 8 The RDA for vitamin C is 75 mg for women 19 years or older and teen boys. Pregnant women need 85 mg/day and lactating women need 120 mg/day. Teen girls need 65 mg/day, men 19 and older need 90 mg/day, and smokers need an extra 35 mg daily. The UL for vitamin C is 2000.13
Thiamin
Thiamin (Vitamin B1) is an essential coenzyme in the metabolism of pyruvate, the end product of glycolysis, and the master fuel input of energy in Krebs’ cycle.7, 8 Other key functions of thiamin are its role in cell respiration, RNA and DNA formation, protein catabolism, growth, appetite, normal muscle tone, and digestive and neurologic functioning.7, 8 Sources of thiamin are found in organ and lean meats, pork, grains, wheat germ, eggs, dried legumes, seeds, and fortified cereals.
The main symptom of thiamin deficiency is beriberi, characterized by a lack of appetite, weakness, and swollen feet or legs.7, 8 Other signs of deficiency include weight loss, mental confusion, and tachycardia.7, 8
Health conditions at risk include those suffering from malnutrition, severe alcoholism, cancer, celiac disease, cardiomyopathies, increased basal metabolic rate, and antibiotic overuse.7, 8 Thiamin toxicity can lead to respiratory failure and death when doses surpass the tolerable upper intake, with noted symptoms of headache, convulsions, muscular weakness, cardiac arrhythmia, and allergic reactions.7, 8
The DRIs for thiamin include AIs for infants as found in human milk; RDAs are based on levels of energy intake with 1.2 mg/day for men and 1.1 mg/day for women.9 No UL has been established.9
Riboflavin
Riboflavin (Vitamin B2) is the main coenzyme in redox reactions of fatty acids and is involved in all macronutrients metabolic reactions to aid in cell respiration and energy formation.7, 8
Other roles of riboflavin are in the maintenance of mucous membranes, and the proper functioning of niacin and pyridoxine.7, 8
Sources of riboflavin are found in milk, yogurt, cheese, egg whites, liver, beef, chicken, fish, legumes, peanuts, enriched grains, and fortified cereals.
The most notable symptom of riboflavin deficiency is growth failure and cheilosis (fissures and scaling of lips). This leads to angular stomatitis (mouth sores), sore throat, and glossitis (magenta, swollen tongue).7, 8
Populations at risk for deficiency are those living in developing countries, those with severe alcoholism, cancers, drug use, and hormone imbalances.7, 8 Riboflavin toxicity is extremely rare. The DRIs for riboflavin include AIs for infants and RDAs based on the amount required to maintain normal tissue reserves, RDA is 1.3 mg/day for men and 1.1 mg/day for women, and no UL has been established.9
Niacin
Niacin (Vitamin B3, Nicotinic acid, Nicotinamide) serves as a coenzyme in the metabolism of carbohydrates, protein, and fat and has an important role in DNA repair and gene stability.7, 8 The precursor of niacin is tryptophan, an essential amino acid, thus, niacin is mainly found in protein sources such as organ meats, poultry, saltwater fish, peanuts and legumes, enriched bread, and fortified cereals.
Signs of niacin deficiency include inflammation and swelling of the oral mucosa, esophagitis, diarrhea, headaches, insomnia, depression, anxiety, tremors, loss of motor function leading to numbness, and paresthesia in limbs. Severe niacin deficiency can lead to pellagra, a disease characterized by dermatitis, diarrhea, dementia, and death if left untreated (the three Ds of pellagra).7, 8
Niacin toxicity is rare; however, cases reported include symptoms of hives, rash (“niacin flush”), excessive sweating, blurred vision, and liver damage. 7, 8 Intake for infants is established as AIs, RDA is 16 mg/day for men and 14 mg/day for women, and UL is 35 mg/day for men and women.9
Pantothenic Acid
Pantothenic Acid (Vitamin B5) serves as a coenzyme in the energy synthesis of fatty acid metabolism. Pantothenic acid is available in all organic forms both in plant and animal tissues, the most important being organ meats, grains, legumes, egg yolks, milk, and sweet potatoes.
Deficiency of pantothenic acid is rare, but signs can include impaired lipid synthesis and energy production leading to nerve weakness and burning sensations in the feet, depression, fatigue, insomnia, and weakness. Toxicity is also rare, with excess B5 causing mild intestinal distress or diarrhea.7, 8 AI for adult men and women is 5 mg/day. UL is not established.9
Pyridoxine
Pyridoxine (Vitamin B6) is a coenzyme in amino acid metabolism and is known for its role in gene expression and hemoglobin synthesis. Pyridoxine can be found in organ meats, fortified cereals, legumes, and nuts. Signs of pyridoxine deficiency are rare but may present as anemia, confusion, irritability, peripheral neuropathies, glossitis, and dermatitis. In addition, toxicity is relatively low, with symptoms reported as limited peripheral sensations, and muscle incoordination.7, 8 The DRIs for vitamin B6 include AIs for infants. Infants need three times as much vitamin B6 as adults. RDA is 1.3–1.7 mg/day for men and 1.3–1.5 mg/day for women. The UL is established at 100 mg/day for adult men and women.9
Biotin
Biotin (Vitamin B7) is a coenzyme in fatty acid synthesis, and carbohydrate metabolism, and plays an important role in converting pyruvic acid to oxaloacetate to initiate the Krebs cycle.7, 8 Sources of biotin are present in organ meats, pork, egg yolk, cereals, legumes, and nuts.
Similar to vitamin K, biotin is the only water-soluble vitamin that is synthesized by gut bacteria. The deficiency of biotin is identified by signs of inflammation on the skin and lips, dermatitis, alopecia, paralysis, depression, nausea, and glossitis. In contrast, there are no known toxic effects if supplementation exceeds upper tolerable limits. The RDA is 30 mg/day for adult men and women, and no UL has been established.9
Folate
Folic Acid (Vitamin B9, Folate) is primarily known for its role in DNA synthesis and red blood cell formation in the bone marrow and is used to prevent neural tube defects in pregnancy.7, 8 Folate is naturally found in food including fortified cereals, lentils and beans, organ meats, citrus fruits, and green leafy vegetables; whereas folic acid is the supplemental form and can be found in fortified foods.
The typical manifestation of folate deficiency is anemia followed by diarrhea, fatigue, irritability, and dyspnea. Populations at risk of deficiency include pregnant women, individuals with malabsorption syndromes, alcoholics, teens, and elderly individuals. Neural tube defects such as spina bifida or anencephaly may result when women are folate deficient during the early months of pregnancy.
There are no reports of toxicity or adverse effects associated with excess intake of folate, although recurrent use can mask vitamin B12 deficiency symptoms.7, 8 Vitamin B12 deficiencies have been linked to Alzheimer’s disease. The DRI is described as AIs for infants. RDA is 400 mcg/day for adults, pregnant women need 600 mcg/day and lactating women need 500 mcg/day. The UL is 1000 mcg/day.9
Cyanocobalamin
Cyanocobalamin (Vitamin B12, Cobalamin) plays an important role as a coenzyme in protein synthesis and the formation of red blood cells. It is attached to intrinsic factors in the stomach and is only absorbed when it reaches the ileum, the main site for fat-soluble vitamin absorption. Vitamin B12 is mainly found in products of animal origin such as organ meats, eggs, fish, and dairy.
Similar to folate, Vitamin B12 deficiency also manifests with anemia, followed by constipation, poor balance, loss of appetite, and numbness and tingling in extremities. Individuals with poor diets, strict vegetarians, senior citizens, and those with severe chronic malnutrition are at high risk for this deficiency.7, 8 Vitamin B12 toxicity has not been reported. The RDA is 2.4 mcg for adults. Pregnant women need 2.6 ug and lactating women need 2.8 ug. No UL was established.9
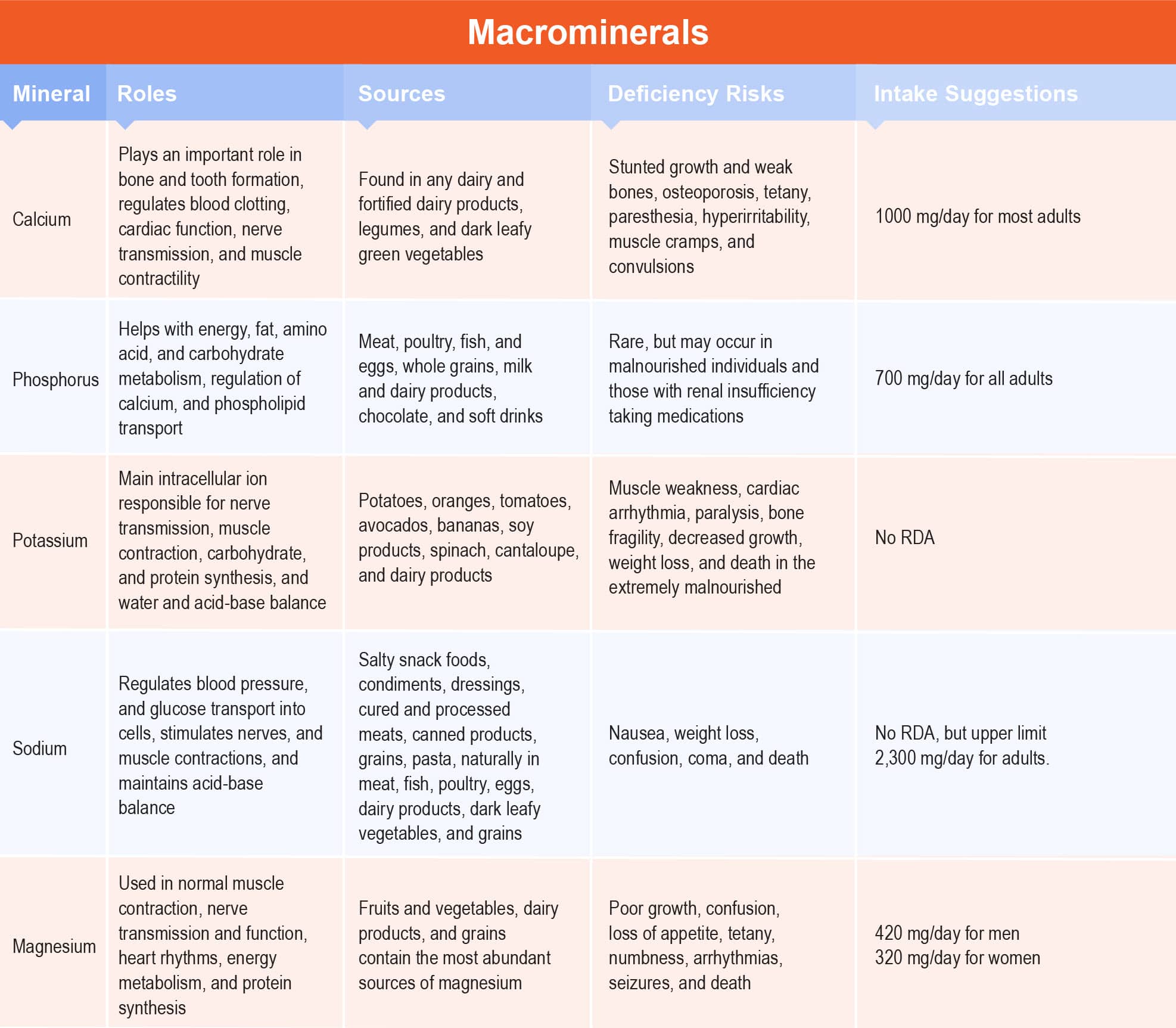
Minerals: Functions, Sources, Intake Guidelines, and Deficiencies
Macrominerals
Calcium
Calcium is one of the most abundant minerals in the body and plays an important role in bone and tooth formation. Additionally, calcium is an intracellular cation that regulates blood clotting, cardiac function, nerve transmission, and muscle contractility. Calcium is found in any dairy and fortified dairy products, legumes, and dark leafy green vegetables. Signs of deficiency (hypocalcemia) manifest in children as stunted growth and weak bones. In adults, calcium deficiency can lead to osteoporosis (bone loss), tetany, paresthesia, hyperirritability, muscle cramps, and convulsions.7, 8 Signs of toxicity (hypercalcemia) usually occur in milk-alkali syndrome, kidney stones, or renal insufficiency. Calcium absorption tends to decrease with increased age for both men and women, so bone health maintenance must be accomplished with vitamin D along with calcium supplementation.7, 8 The RDA for calcium is 1000 mg/day for most adults (19–50 year-old men and women; 51–70 year-old men), 1300 mg for teenagers, and 1200 mg for those over 50 years. The UL is 2,500 mg/day (19–50 years) and 2,000 mg/day (>50 years).9
Phosphorus
Phosphorus is the second most abundant mineral after calcium and plays a vital role in energy, fat, amino acid, and carbohydrate metabolism, regulation of calcium, and phospholipid transport.7, 8 Phosphorus intake can be achieved with virtually any food and is abundant in protein-rich foods such as meat, poultry, fish, and eggs, whole grains, milk and dairy products, chocolate, and soft drinks.
Phosphorus deficiency (hypophosphatemia) is rare but may occur in malnourished individuals and those with renal insufficiency taking medications. Toxicity (hyperphosphatemia) is not common but can promote paralysis, muscular weakness, arrhythmias, heart disturbances, and even death if it occurs.7, 8 The RDA for adult men and women is 700 mg/day, and UL for adults varies from 3–4 g/day.9
Potassium
Potassium is known as the main intracellular ion responsible for nerve transmission, muscle contraction, carbohydrate, and protein synthesis, and water and acid-base balance. Food sources high in potassium include potatoes, oranges, tomatoes, avocados, bananas, soy products, spinach, cantaloupe, and dairy products.
Signs of deficiency (hypokalemia) include muscle weakness, cardiac arrhythmia, paralysis, bone fragility, decreased growth, weight loss, and even death, which is often seen in malnourished individuals.7, 8 Excess potassium (hyperkalemia) can lead to paralysis, muscular weakness, arrhythmias, heart disturbances, and even death. For potassium, there are no specific RDA, AI, or UL.9
Sodium
Sodium is the main extracellular ion along with chloride and its main function is to regulate blood pressure, and glucose transport into cells, to stimulate nerves, and muscle contractions, and to maintain acid-base balance.7, 8
Sodium is found in many processed foods in the American diet such as salty snack foods, condiments, and dressings, cured and processed meats, canned products, grains, and pasta. Natural sources include meat, fish, poultry, eggs, dairy products, dark leafy vegetables, and grains. Sodium deficiency (hyponatremia) can occur from water overload, resulting in nausea, weight loss, confusion, coma, and even death.7, 8
Excess sodium (hypernatremia) is often seen in individuals with dehydration, malnutrition, and severe weight loss, and can lead to symptoms of confusion, high blood pressure, heart failure, and coma.7, 8 There is no specific RDA set for sodium, the UL is 2,300 mg/day for adults.9
Magnesium
Magnesium is an essential mineral used by more than half of the cells in our body in processes such as normal muscle contraction, nerve transmission and function, heart rhythms, energy metabolism, and protein synthesis. Magnesium is present in most foods. Fruits and vegetables, dairy products, and grains contain the most abundant sources of magnesium.
Signs of deficiency (hypomagnesemia) can occur in malnourished individuals and lead to poor growth, confusion, loss of appetite, tetany, numbness, arrhythmias, seizures, and even death.
Excess magnesium (hypermagnesemia) can be seen with kidney failure, and cause nausea, osmotic diarrhea, appetite loss, muscle weakness, respiratory failure, extremely low blood pressure, and irregular heartbeat.7, 8 The RDA is typically 420 mg for men and 320 mg for women. UL for supplemental magnesium for adolescents and adults is 350 mg/d.9
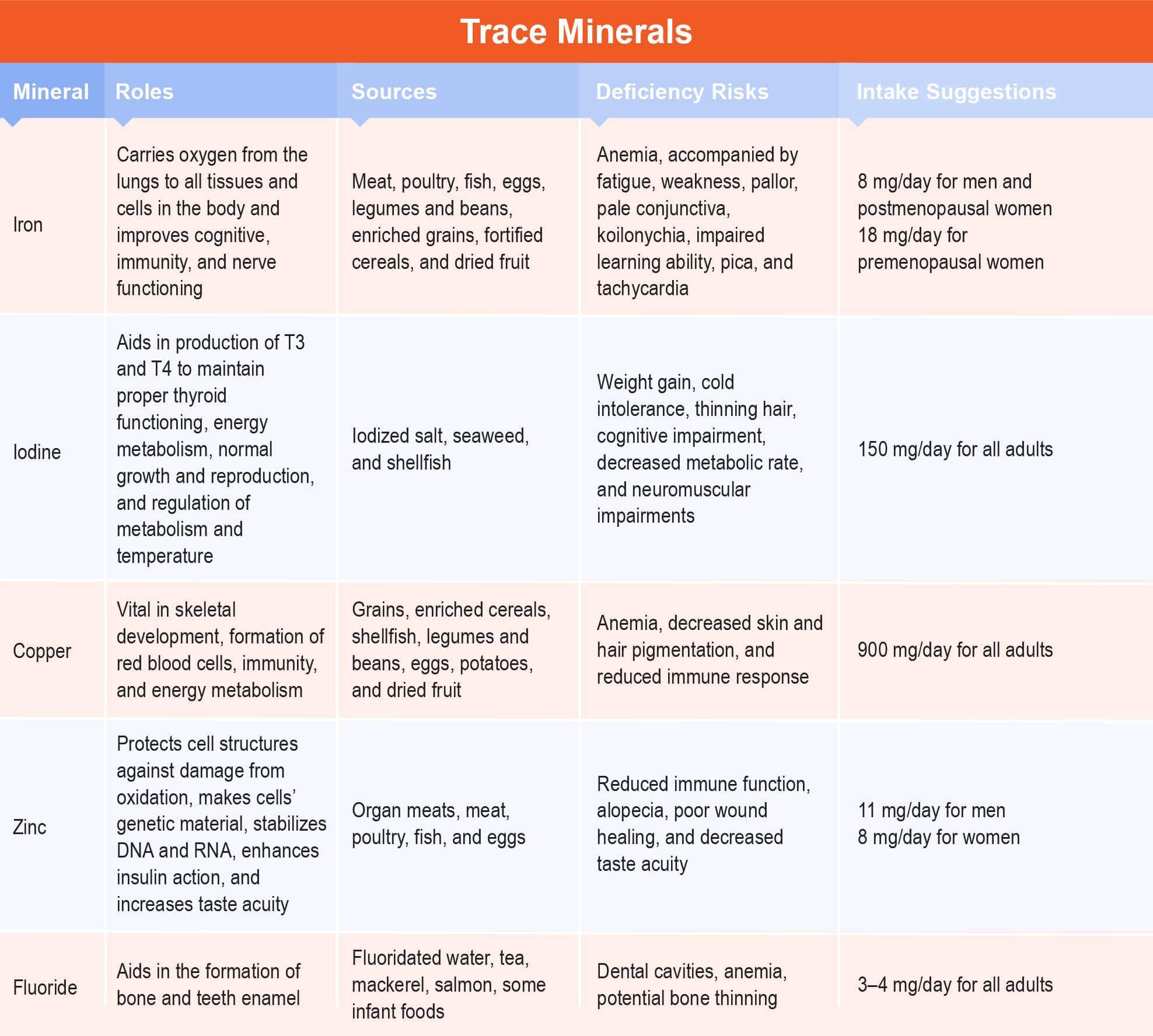
Trace Minerals
Iron
Iron is the most abundant trace mineral, existing in all animal and plant cells. Functional iron is composed of two proteins: hemoglobin in red blood cells and myoglobin in muscle cells.7, 8 The main function of iron is to carry oxygen from the lungs to all tissues and cells in the body and improve cognitive, immunity, and nerve functioning.7, 8 The food sources rich in iron include meat, poultry, fish, eggs, legumes and beans, enriched grains, fortified cereals, and dried fruit.
The most notable sign of iron deficiency is anemia, accompanied by fatigue, weakness, pallor, pale conjunctiva, koilonychia (thin, spoon-shaped nails), impaired learning ability, pica, and tachycardia.7, 8 Iron toxicity can occur from taking iron supplements daily or recurrent transfusions, and commonly manifests with vomiting, diarrhea, GI distress, and drowsiness.7, 8
The RDA is 8 mg for men and postmenopausal women; 18 mg for premenopausal women. Pregnant women need 27 mg/d and breastfeeding women need 9 mg.9 Teenage girls (ages 14–18 years) need 15 mg of iron per day (27 mg if pregnant; 10 mg if breastfeeding). Teenage boys (ages 14–18 years) need 11 mg of iron per day. The UL for iron is 45 mg/d.9
Iodine
Iodine (Iodide) is part of the hormone thyroxine and aids in the production of T3 and T4 to maintain proper thyroid functioning, energy metabolism, in normal growth and reproduction, and the regulation of metabolism and temperature. Iodine can be found in iodized salt, seaweed, and shellfish. Iodine deficiency and excess can both cause an enlarged thyroid gland. Deficiency is often associated with weight gain, cold intolerance, thinning hair, cognitive impairment, decreased metabolic rate, and neuromuscular impairments.7, 8 The RDA is 150 mg/d for both men and women. UL is 1.1 mg/day.9
Copper
Copper is an antioxidant that is vital in skeletal development, formation of red blood cells, immunity, and energy metabolism.7, 8 Copper is mainly found in grains, enriched cereals, shellfish, legumes and beans, eggs, potatoes, and dried fruit. Copper deficiency is rare in adults, except in individuals with celiac disease. Symptoms of deficiency include anemia, decreased skin and hair pigmentation, and reduced immune response.7, 8 Copper toxicity is also rare, but can occur in individuals with liver disease, leading to copper deposits in the brain, diarrhea, tremors, and liver damage.7, 8 The RDA is 900 mg daily for men and women and UL is established at 10 mg/d.9
Zinc
Zinc is present in very small quantities in the body and its main function is to protect cell structures against damage from oxidation, make cells’ genetic material, stabilize DNA and RNA, enhance insulin action, and increase taste acuity.7, 8 Zinc is found in most protein foods like organ meats, meat, poultry, fish, and eggs. Deficiency is not common in developing countries, but when it occurs it can lead to reduced immune function, alopecia, poor wound healing, and decreased taste acuity (hypogeusia).7, 8 Signs of zinc excess include vomiting, diarrhea, headaches, and exhaustion. The RDA is 11 mg for men and 8 mg for women. UL is 40 mg.9
Fluoride
Fluoride is the most abundant mineral in water and soil that aids in the formation of bone and teeth enamel. Sources of fluoride include fluoridated water, tea, mackerel, salmon, and some infant foods. Signs of deficiency include dental cavities, anemia, and potential bone thinning, and toxicity may lead to tooth mottling and discoloration, and neurological problems.7, 8 The RDA is 3–4 mg/d for men and women. UL is set at 10 mg/d.9
Summary
Micronutrients play many vital roles in basic biological functions as well as responses and adaptations to exercise.
With a working knowledge of micronutrients, fitness professionals are better prepared to identify potential symptoms of deficiency or overdose and refer the client to an appropriate healthcare provider.
Making specific diagnoses or recommendations is outside the Trainer Academy CPT Scope of Practice.
References
- Centers for Disease Control and Prevention. Micronutrient facts. Available at: https://www.cdc.gov/nutrition/micronutrient-malnutrition/micronutrients/index.html. Published February 1, 2022. Accessed September 26, 2022.
- Muñoz García M, Pérez Menéndez-Conde C, Bermejo Vicedo T. Avances en el conocimiento del uso de micronutrientes en nutrición artificial [Advances in the knowledge of the use of micronutrients in artificial nutrition]. Nutr Hosp. 2011;26(1):37-47
- Stipanuk, M. H. Biochemical, physiological, & molecular aspects of human nutrition. 3rd ed. St. Louis: Saunders Elsevier; 2006.
- Shenkin A. Micronutrients in health and disease. Postgrad Med J. 2006;82(971):559-567. https://doi.org/10.1136/pgmj.2006.047670
- Rizvi S, Raza ST, Ahmed F, Ahmad A, Abbas S, Mahdi F. The role of vitamin e in human health and some diseases. Sultan Qaboos Univ Med J. 2014;14(2):e157-e165.
- Demling RH, DeBiasse MA. Micronutrients in critical illness [published correction appears in Crit Care Clin 1996 Oct;12(4): xi]. Crit Care Clin. 1995;11(3):651-673.
- Sizer FS, Whitney E. Nutrition Concepts & Controversies. 13th ed. Belmont, CA: Wadsworth Publishing Co; 2014
- Escott-Stump S. Nutrition & Diagnosis-Related Care. Academy of Nutrition and Dietetics; 2022.
- National Institutes of Health, Office of Dietary Supplements. Nutrient Recommendations: Dietary Reference Intakes (DRI). Available at: https://ods.od.nih.gov/Health_Information/Dietary_Reference_Intakes.aspx. Accessed September 26, 2022.
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans, 2020-2025. 2020. 9th Edition. https://www.dietaryguidelines.gov
- National Institutes of Health. Vitamin D. Available at: https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/ Published February 11, 2016. Accessed September 26, 2022.